Introduction to Von Hippel-Lindau Disease
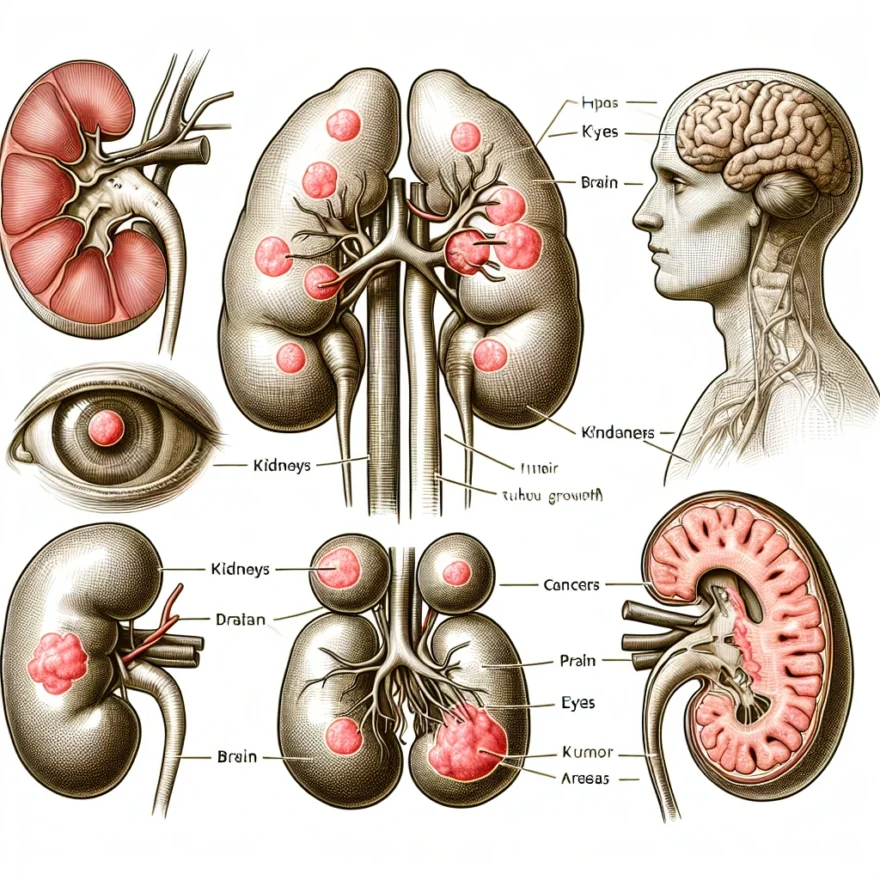
Von Hippel-Lindau Disease, commonly known as VHL, is a rare, inherited multi-system disorder characterized by the formation of tumors and cysts in many different parts of the body. These growths can occur in the central nervous system (including the brain and spinal cord), the kidneys, pancreas, adrenal glands, inner ears, eyes, reproductive organs, and more. The tumors can be either benign (noncancerous) or malignant (cancerous).
Named after the two German ophthalmologists who first described it in the early 20th century, Eugen von Hippel and Arvid Lindau, VHL is a condition that affects about 1 in 36,000 people. It does not discriminate, affecting individuals across all ethnicities and genders. The onset of symptoms typically begins in adulthood, although it can also present in children.
The tumors associated with VHL are highly vascular, meaning they have a large number of blood vessels. This is because the gene mutation associated with VHL disrupts the body’s ability to control angiogenesis, the process by which new blood vessels are formed. As a result, the body overproduces blood vessels in certain areas, leading to the formation of tumors and cysts.
While the disease is chronic and life-long, the severity and progression of VHL can vary greatly from person to person, even among members of the same family. Some people may live most of their lives with minimal symptoms, while others may experience serious complications. The wide range of symptoms and health problems associated with VHL can make it challenging to diagnose and manage, requiring a multidisciplinary approach to care.
Despite its rarity and complexity, significant advances have been made in understanding and treating VHL in recent years. With early detection and regular monitoring, many of the complications associated with VHL can be managed effectively, enabling individuals with the condition to lead active, productive lives.
Table of contents
- Introduction to Von Hippel-Lindau Disease
- The Genetic Aspect of Von Hippel-Lindau Disease
- How Von Hippel-Lindau Disease Affects Multiple Organs
- Symptoms of Von Hippel-Lindau Disease
- Diagnosis of Von Hippel-Lindau Disease
- Treatment Options for Von Hippel-Lindau Disease
- Living with Von Hippel-Lindau Disease
- The Role of Family and Caregivers in Managing Von Hippel-Lindau Disease
- Recent Advancements in Von Hippel-Lindau Disease Research
- Common Questions and Answers about Von Hippel-Lindau Disease
The Genetic Aspect of Von Hippel-Lindau Disease
Von Hippel-Lindau (VHL) disease is a rare, genetic multi-system disorder characterized by the formation of tumors in several organs. These tumors can be benign or malignant and are often associated with cysts. VHL disease is caused by mutations in the VHL gene, which is located on the short arm (p) of chromosome 3 (3p25-26).
The VHL gene is known as a tumor suppressor gene. It produces a protein that plays a key role in the body’s natural defense against the uncontrolled growth of cells, which can lead to the formation of tumors. This protein regulates the activity of other genes and plays a crucial role in many cellular processes, including the response to changes in oxygen levels. When functioning normally, the VHL protein helps to prevent the growth of tumors by targeting hypoxia-inducible factor (HIF) for degradation. HIF is a protein that triggers the growth of new blood vessels when tissues are deprived of oxygen, a process known as angiogenesis. Angiogenesis is a normal process in wound healing and in the formation of the placenta during pregnancy. However, it also plays a critical role in the growth of cancer.
When mutations occur in the VHL gene, the VHL protein is not produced or does not function properly. As a result, HIF is not broken down and accumulates in cells. This accumulation stimulates the production of certain genes that promote cell division and blood vessel formation, leading to the development of tumors and cysts in multiple organs of the body.
VHL disease is inherited in an autosomal dominant manner, which means that an affected person has a 50% chance of passing the disorder to each of their offspring. Most people with VHL disease inherit an altered copy of the gene from a parent who has the disorder. However, approximately 20% of cases result from new mutations in the gene and occur in people with no history of the disorder in their family.
Genetic testing is available for individuals who may be at risk for VHL disease. This testing can identify mutations in the VHL gene that cause the disorder. Genetic counseling is recommended for individuals and families who are considering genetic testing for VHL disease.
How Von Hippel-Lindau Disease Affects Multiple Organs
Von Hippel-Lindau Disease (VHL) is a rare genetic disorder that affects multiple organs in the body. It is caused by mutations in the VHL gene, which is responsible for suppressing tumor growth. When this gene is mutated, it leads to the development of tumors in various organs.
One of the organs commonly affected by VHL is the central nervous system. Tumors, known as hemangioblastomas, can develop in the brain and spinal cord. These tumors can cause symptoms such as headaches, dizziness, problems with coordination, and even seizures. If left untreated, these tumors can grow larger and potentially compress vital structures in the central nervous system.
In addition to the central nervous system, VHL can also affect the eyes. Retinal hemangioblastomas, or tumors in the retina, can lead to vision problems or even loss of vision if they are not treated. These tumors can be detected during routine eye examinations and can be managed through treatments such as laser therapy or cryotherapy.
VHL can also impact the kidneys, leading to the development of renal cell carcinoma (kidney cancer). These tumors can vary in size and aggressiveness, and if left untreated, they can spread to other parts of the body. Regular monitoring through imaging studies is crucial to detect any kidney tumors early and determine the appropriate course of treatment.
The pancreas is another organ that can be affected by VHL. Tumors called pancreatic neuroendocrine tumors (PNETs) can develop, which can cause symptoms such as abdominal pain, weight loss, and changes in blood sugar levels. Treatment options for PNETs depend on the size and location of the tumors, and may include surgery, medication, or other targeted therapies.
VHL can also lead to the development of tumors in the adrenal glands, which are responsible for producing hormones that regulate various bodily functions. These tumors, known as pheochromocytomas, can cause symptoms such as high blood pressure, rapid heartbeat, and excessive sweating. Treatment for pheochromocytomas typically involves surgical removal of the tumor.
Furthermore, VHL can affect other organs such as the liver, lungs, and reproductive organs, although these occurrences are less common. Liver cysts and tumors, lung cysts, and tumors in the female reproductive system can occur in individuals with VHL. Regular screenings and imaging studies are important to detect any abnormalities in these organs.
It is important to note that the severity and specific manifestations of VHL can vary among individuals. Some may only develop tumors in one organ, while others may experience tumors in multiple organs. Regular medical follow-ups and screenings are essential for early detection and management of any tumors that may arise.
Symptoms of Von Hippel-Lindau Disease
Von Hippel-Lindau Disease (VHL) is a rare genetic disorder that can cause the development of tumors in multiple organs throughout the body. These tumors, known as hemangioblastomas, can occur in various locations such as the brain, spinal cord, kidneys, adrenal glands, pancreas, and other organs.
The symptoms of Von Hippel-Lindau Disease can vary depending on the location and size of the tumors. Some individuals may experience no symptoms at all, while others may have a range of symptoms that can significantly impact their quality of life.
One of the most common symptoms of VHL is headaches. These headaches can be severe and persistent, often accompanied by nausea and vomiting. The headaches may be caused by the presence of hemangioblastomas in the brain or spinal cord, which can exert pressure on surrounding tissues.
Another common symptom is vision problems. Hemangioblastomas in the eyes can lead to blurry or distorted vision, or even partial or complete loss of vision. These tumors can affect the retina, optic nerve, or other structures in the eye, leading to visual impairment.
Individuals with VHL may also experience problems with balance and coordination. This can be due to the presence of tumors in the cerebellum, which is responsible for coordinating movement and maintaining balance. Difficulties with walking, dizziness, and a lack of coordination are common symptoms in these cases.
Renal cell carcinoma, a type of kidney cancer, is also associated with VHL. This can cause symptoms such as blood in the urine, abdominal pain, and a palpable mass in the abdomen. Additionally, individuals with VHL may develop cysts in the kidneys, which can lead to kidney dysfunction and high blood pressure.
Other symptoms of VHL can include abdominal pain, nausea, vomiting, and digestive problems. These symptoms may be indicative of tumors in the pancreas or other abdominal organs. Adrenal gland tumors can also cause hormonal imbalances, leading to symptoms such as high blood pressure, rapid heartbeat, and excessive sweating.
It is important to note that the symptoms of VHL can vary greatly from person to person, and not all individuals with the condition will experience the same symptoms or have tumors in the same organs. Regular medical check-ups and screenings are crucial for early detection and management of VHL-related symptoms.
If you or a loved one are experiencing any of these symptoms, especially in combination with a family history of VHL, it is important to consult with a healthcare professional for further evaluation and diagnosis.
Diagnosis of Von Hippel-Lindau Disease
Von Hippel-Lindau Disease (VHL) is a genetic disorder that predisposes individuals to the development of tumors in multiple organs. Due to its hereditary nature, early diagnosis is crucial for effective management and treatment of the disease.
Diagnosing VHL involves a comprehensive evaluation of an individual’s medical history, physical examination, and various diagnostic tests. The process typically begins with a thorough discussion with the patient to identify any family history of VHL or related symptoms.
Genetic testing plays a significant role in diagnosing VHL. This involves analyzing a blood sample to identify mutations in the VHL gene. As VHL is caused by mutations in this gene, genetic testing can confirm the presence of the disease and determine if an individual has inherited the faulty gene.
In addition to genetic testing, imaging studies are crucial for identifying and monitoring tumors associated with VHL. Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) scans are commonly used to visualize tumors in the brain, spinal cord, kidneys, adrenal glands, and other affected organs. These imaging techniques provide detailed images that help in determining the size, location, and characteristics of the tumors.
Ophthalmologic examinations are also an important part of the diagnostic process for VHL. The presence of retinal hemangioblastomas, which are characteristic tumors associated with VHL, can be detected through a comprehensive eye examination. This may involve dilating the pupils and using specialized equipment to examine the retina.
Once a diagnosis of VHL is confirmed, regular monitoring and follow-up examinations are necessary to detect and manage the growth of tumors. This may involve periodic imaging studies, ophthalmologic examinations, and other tests to assess the progression of the disease.
It is important to note that the diagnosis of VHL can have significant implications for both the individual and their family members. Genetic counseling is often recommended to help individuals understand the inheritance pattern of VHL, assess the risk of passing the condition to future generations, and make informed decisions regarding family planning.
Overall, the diagnosis of Von Hippel-Lindau Disease involves a multidisciplinary approach, combining genetic testing, imaging studies, and ophthalmologic examinations. Early detection and ongoing monitoring are essential for effective management and treatment of the disease, allowing for timely intervention and improved outcomes.
Treatment Options for Von Hippel-Lindau Disease
Von Hippel-Lindau Disease (VHL) is a rare genetic disorder that predisposes individuals to the development of tumors in multiple organs. The treatment options for VHL vary depending on the location, size, and aggressiveness of the tumors. The main goals of treatment are to control tumor growth, manage symptoms, and prevent complications.
1. Surgery:
Surgery is often the primary treatment option for VHL, especially when tumors are localized and accessible. The surgical approach depends on the specific organ affected and the size of the tumor. Surgeons may opt for partial or complete removal of the tumor, depending on the situation. In some cases, minimally invasive techniques such as laparoscopy or robotic surgery can be used, which result in smaller incisions, reduced pain, and faster recovery times.
2. Radiation Therapy:
Radiation therapy may be used to treat VHL tumors that cannot be surgically removed or to control tumor growth in cases where surgery is not feasible. This treatment uses high-energy beams to target and destroy cancer cells. It can be delivered externally (external beam radiation) or internally (brachytherapy) depending on the location and size of the tumor. Radiation therapy is often used in combination with surgery or other treatments to achieve the best possible outcome.
3. Medications:
Medications can be used to manage symptoms and slow down the growth of VHL tumors. For example, medications called tyrosine kinase inhibitors (TKIs) can be prescribed to inhibit the growth of blood vessels that supply nutrients to the tumors. These medications can help shrink tumors and prevent new ones from forming. Other medications may be prescribed to manage specific symptoms or complications associated with VHL, such as pain or high blood pressure.
4. Surveillance and Monitoring:
Regular surveillance and monitoring are crucial for individuals with VHL to detect and manage tumors at an early stage. This involves periodic imaging tests such as MRI, CT scans, or ultrasound to monitor the size and growth of tumors. Depending on the findings, treatment options can be adjusted accordingly. Surveillance is typically tailored to each individual based on their specific VHL manifestations and medical history.
5. Clinical Trials:
Participating in clinical trials can be an option for individuals with VHL who are seeking innovative treatments or therapies that are not yet widely available. Clinical trials help researchers evaluate the safety and effectiveness of new treatments or combinations of treatments. It is important to discuss the potential benefits and risks of participating in a clinical trial with a healthcare professional.
It is important to note that the choice of treatment for VHL should be individualized and based on the specific needs and circumstances of each patient. A multidisciplinary approach involving a team of healthcare professionals, including geneticists, oncologists, surgeons, and other specialists, is often necessary to provide comprehensive care and optimize treatment outcomes.
Living with Von Hippel-Lindau Disease
Von Hippel-Lindau Disease (VHL) is a rare genetic disorder that can affect multiple organs in the body. Living with VHL can present various challenges, both physical and emotional, for individuals and their families. It is important to understand how to manage the disease and maintain a good quality of life.
Regular Medical Monitoring
Individuals with VHL should undergo regular medical monitoring to detect and manage any tumor growth or complications. This typically involves frequent imaging scans, such as MRI or CT scans, to monitor the organs affected by VHL. Regular check-ups with specialists, such as neurologists, ophthalmologists, and oncologists, are also essential to ensure early detection and appropriate treatment.
Adopting a Healthy Lifestyle
Living with VHL requires adopting a healthy lifestyle to minimize the risk of complications. This includes maintaining a balanced diet, engaging in regular exercise, and avoiding smoking and excessive alcohol consumption. A healthy lifestyle can help strengthen the immune system, improve overall well-being, and potentially reduce the risk of tumor growth.
Managing Symptoms and Complications
Individuals with VHL may experience various symptoms and complications depending on the organs affected by the disease. It is important to work closely with healthcare professionals to manage these symptoms effectively. This may involve medication to control blood pressure, pain management strategies, or surgical interventions to remove tumors or address specific complications.
Emotional Support
Living with a chronic condition like VHL can be emotionally challenging. It is important for individuals and their families to seek emotional support, whether through support groups, counseling, or connecting with others who have VHL. Sharing experiences, concerns, and coping strategies can provide valuable emotional support and help individuals navigate the emotional impact of the disease.
Family Planning and Genetic Counseling
For individuals with VHL who are planning to start a family, genetic counseling is crucial. Genetic counselors can provide information about the risk of passing on the VHL gene to children and discuss reproductive options. Family planning decisions should be made in consultation with healthcare professionals to ensure the best possible outcomes.
Regular Communication with Healthcare Team
Maintaining open and regular communication with the healthcare team is essential for individuals with VHL. This includes sharing any changes in symptoms, concerns, or questions about treatment options. Staying informed and actively participating in the management of the disease can help individuals feel empowered and confident in their healthcare decisions.
Support from Family and Caregivers
Living with VHL can be challenging, and having a strong support system is crucial. Family members and caregivers play a vital role in providing physical and emotional support. They can assist with daily activities, accompany individuals to medical appointments, and offer a listening ear during difficult times. Open communication and understanding within the family unit can help alleviate some of the burdens associated with VHL.
Seeking Second Opinions
Given the complexity of VHL and the potential impact on multiple organs, seeking second opinions from specialists can be beneficial. Second opinions can provide additional perspectives on treatment options and help individuals make informed decisions about their healthcare. It is important to find healthcare professionals who are experienced in managing VHL and have access to the latest research and treatment advancements.
Participating in Research and Clinical Trials
Individuals with VHL may consider participating in research studies and clinical trials. These opportunities can contribute to the advancement of knowledge and potential treatment options for VHL. It is important to discuss participation in research with healthcare professionals to understand the potential risks and benefits.
Living with Von Hippel-Lindau Disease requires a comprehensive approach that includes regular medical monitoring, adopting a healthy lifestyle, managing symptoms and complications, seeking emotional support, and maintaining open communication with healthcare professionals. With proper management and support, individuals with VHL can lead fulfilling lives and effectively navigate the challenges associated with the disease.
The Role of Family and Caregivers in Managing Von Hippel-Lindau Disease
The Role of Family and Caregivers in Managing Von Hippel-Lindau Disease
Von Hippel-Lindau Disease (VHL) is a rare genetic disorder that can have a significant impact on the lives of those affected. While the individual with VHL is the primary focus of medical attention, it is essential to recognize the crucial role that family members and caregivers play in managing the disease.
Family members and caregivers provide emotional support, assist with daily activities, and help navigate the complex medical journey that comes with VHL. Their involvement can greatly contribute to the overall well-being and quality of life for individuals with VHL.
Here are some key ways in which family members and caregivers can make a difference:
- Education and Awareness: Family members and caregivers can educate themselves about VHL, its symptoms, treatment options, and potential complications. This knowledge will enable them to better understand the challenges faced by their loved ones and provide appropriate support.
- Emotional Support: Dealing with a chronic illness like VHL can be emotionally challenging. Family members and caregivers can offer a listening ear, provide comfort, and be a source of strength during difficult times.
- Assistance with Medical Appointments: VHL often requires frequent medical appointments with various specialists. Family members and caregivers can help schedule appointments, accompany the individual to consultations, and take notes to ensure important information is not missed.
- Medication Management: VHL may involve taking multiple medications. Family members and caregivers can help organize medications, ensure they are taken as prescribed, and keep track of any side effects or changes in symptoms.
- Advocacy: Family members and caregivers can serve as advocates for individuals with VHL, ensuring their needs are met within the healthcare system. They can communicate with healthcare providers, insurance companies, and other relevant parties to ensure the best possible care.
- Supporting Lifestyle Modifications: Certain lifestyle modifications, such as a healthy diet and regular exercise, can help manage VHL symptoms and overall well-being. Family members and caregivers can assist in implementing and maintaining these lifestyle changes.
- Providing a Safe Environment: Individuals with VHL may be more susceptible to certain health risks. Family members and caregivers can create a safe environment by minimizing potential hazards, such as ensuring proper lighting and removing obstacles that may increase the risk of falls.
It is important for family members and caregivers to prioritize their own well-being as well. Taking care of oneself physically and emotionally allows them to better support their loved ones with VHL. Seeking support from support groups, counseling, or respite care can be beneficial in managing the challenges that come with caring for someone with VHL.
By actively participating in the management of VHL, family members and caregivers can make a significant impact on the overall quality of life for individuals with the disease. Their support, understanding, and advocacy are invaluable in helping individuals with VHL navigate their journey and face the challenges that arise.
Recent Advancements in Von Hippel-Lindau Disease Research
Von Hippel-Lindau Disease (VHL) is a complex genetic disorder that predisposes individuals to the development of tumors in multiple organs. Over the years, significant advancements have been made in understanding and managing this condition. Researchers and medical professionals continue to work tirelessly to improve the diagnosis, treatment, and overall outcomes for individuals with VHL.
One of the recent advancements in VHL research is the identification of specific genetic mutations associated with the disease. Scientists have discovered that VHL is caused by mutations in the VHL gene, which plays a crucial role in tumor suppression. By studying these mutations, researchers have gained insights into the molecular mechanisms underlying tumor development in VHL.
Another area of progress is the development of targeted therapies for VHL-associated tumors. Targeted therapies are drugs that specifically target the molecular pathways involved in tumor growth. These therapies have shown promising results in shrinking or stabilizing VHL-related tumors, particularly in the kidneys and central nervous system.
In addition to targeted therapies, researchers are also exploring the potential of immunotherapy in VHL treatment. Immunotherapy harnesses the power of the immune system to recognize and destroy cancer cells. Preliminary studies have shown encouraging results in using immunotherapy to treat VHL-associated tumors, and ongoing clinical trials are further evaluating its effectiveness.
Advancements in imaging technology have also played a crucial role in VHL research. High-resolution imaging techniques, such as magnetic resonance imaging (MRI) and computed tomography (CT), have improved the detection and monitoring of VHL-related tumors. These advanced imaging methods allow for early detection, accurate characterization, and precise monitoring of tumor growth, enabling timely intervention and treatment.
Furthermore, genetic testing has become more accessible and affordable, facilitating early diagnosis and genetic counseling for individuals at risk of VHL. Identifying VHL mutations in at-risk individuals allows for proactive surveillance and management of the disease, potentially leading to better outcomes and improved quality of life.
Collaborative efforts among researchers, medical professionals, and patient advocacy groups have also contributed to the progress in VHL research. The sharing of knowledge, resources, and patient data has accelerated the understanding of VHL and the development of innovative treatment approaches.
It is important to note that while significant advancements have been made, VHL remains a complex and challenging condition. Continued research is essential to further unravel the intricacies of the disease and develop more effective treatment strategies.
Common Questions and Answers about Von Hippel-Lindau Disease
Q: What is Von Hippel-Lindau Disease?
A: Von Hippel-Lindau Disease (VHL) is a rare genetic disorder characterized by the development of tumors in multiple organs of the body. It is caused by mutations in the VHL gene, which is responsible for regulating cell growth and division. These mutations lead to the formation of abnormal blood vessels and the growth of tumors in organs such as the brain, spinal cord, kidneys, adrenal glands, and pancreas.
Q: Can Von Hippel-Lindau Disease be inherited?
A: Yes, Von Hippel-Lindau Disease is an inherited condition. It follows an autosomal dominant pattern of inheritance, which means that a person who inherits a mutated copy of the VHL gene from one parent will develop the disease. Each child of an affected individual has a 50% chance of inheriting the condition.
Q: What are the symptoms of Von Hippel-Lindau Disease?
A: The symptoms of Von Hippel-Lindau Disease vary depending on the location and size of the tumors. Common symptoms include headaches, dizziness, vision problems, high blood pressure, abdominal pain, and changes in urine color or volume. Other symptoms may include back pain, weakness or numbness in the limbs, and hormonal imbalances.
Q: How is Von Hippel-Lindau Disease diagnosed?
A: Von Hippel-Lindau Disease is typically diagnosed through a combination of medical history, physical examinations, and imaging tests such as MRI, CT scans, and ultrasound. Genetic testing can also be conducted to identify mutations in the VHL gene. Regular screenings and monitoring of affected individuals and their family members are crucial for early detection and treatment.
Q: What are the treatment options for Von Hippel-Lindau Disease?
A: The treatment of Von Hippel-Lindau Disease depends on the location and size of the tumors, as well as the individual’s overall health. Treatment options may include surgery to remove tumors, radiation therapy, embolization to block blood flow to the tumors, and targeted drug therapies. Regular monitoring and follow-up care are essential to manage the disease effectively.
Q: Can Von Hippel-Lindau Disease be cured?
A: Currently, there is no cure for Von Hippel-Lindau Disease. However, with early detection, regular screenings, and appropriate treatment, the progression of the disease can be managed, and the symptoms can be controlled. It is important for individuals with VHL to work closely with a medical team specializing in the condition to develop a comprehensive treatment plan.
Q: How does Von Hippel-Lindau Disease affect daily life?
A: Von Hippel-Lindau Disease can have a significant impact on daily life due to the potential development of tumors in multiple organs. The disease requires regular medical appointments, screenings, and treatments. Individuals may experience physical and emotional challenges, and they may need to make adjustments to their lifestyle and career choices. However, with proper management and support, many individuals with VHL are able to lead fulfilling lives.
Q: Are there any support groups or resources available for individuals with Von Hippel-Lindau Disease?
A: Yes, there are several support groups and resources available for individuals and families affected by Von Hippel-Lindau Disease. These organizations provide information, support, and a platform for connecting with others who have the condition. Some notable resources include the VHL Alliance, the National Institutes of Health (NIH), and various online communities dedicated to VHL awareness and support.
Q: What are the recent advancements in Von Hippel-Lindau Disease research?
A: Ongoing research in Von Hippel-Lindau Disease aims to improve our understanding of the condition and develop more effective treatments. Some recent advancements include the identification of potential drug targets for VHL-related tumors, advancements in genetic testing methods, and the exploration of gene therapy approaches. These advancements offer hope for improved outcomes and quality of life for individuals with VHL.
Q: Can Von Hippel-Lindau Disease be prevented?
A: As Von Hippel-Lindau Disease is a genetic condition, it cannot be prevented. However, genetic counseling and testing can help individuals understand their risk of developing the disease and make informed decisions about family planning. Regular screenings and early detection can help manage the disease and minimize its impact on overall health.