Introduction: The Gut-Brain Connection
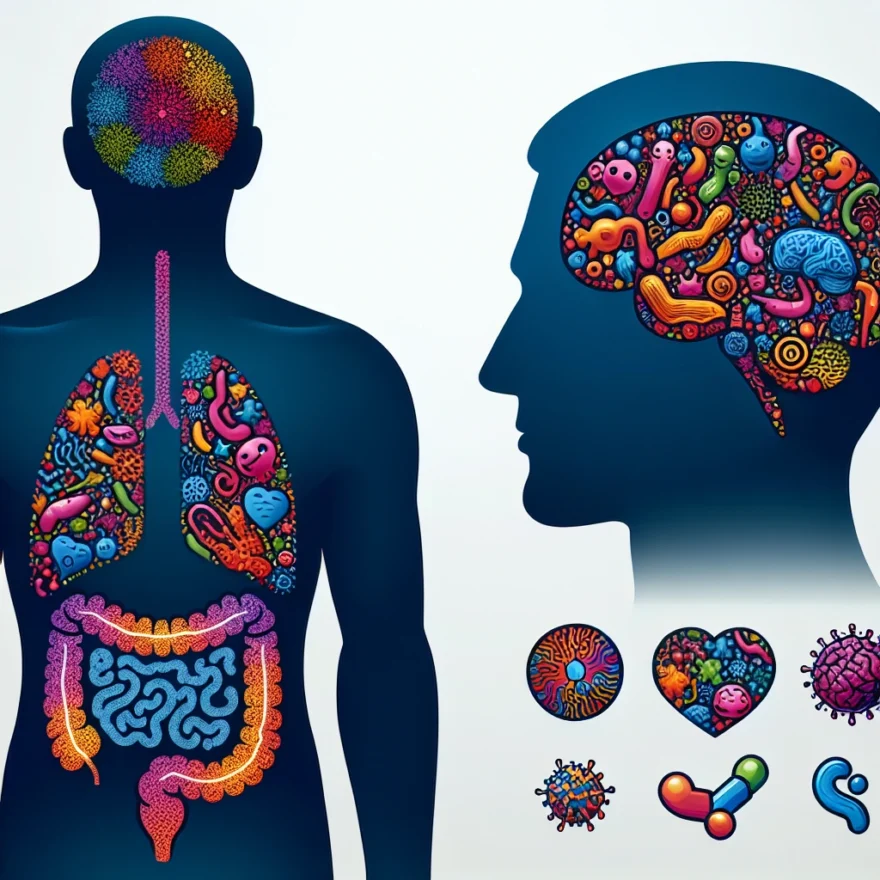
The human body is a complex system of interconnected parts, each playing a vital role in maintaining overall health. One such connection that has recently come under the spotlight is the link between the gut and the brain. This connection, known as the gut-brain axis, is a bidirectional communication system that not only ensures the proper functioning of the gastrointestinal tract but also seems to play a crucial role in our mental health.
Indeed, the gut is often referred to as the ‘second brain’ due to its extensive network of neurons and the production of neurotransmitters, which are chemical messengers that allow neurons to communicate with each other. The gut is home to trillions of bacteria, collectively known as the gut microbiota, which greatly influence the gut-brain axis and, in turn, our mental health.
Emerging research suggests that an imbalance in the gut microbiota, known as dysbiosis, may contribute to the development of mood disorders such as depression and anxiety. This is because the gut microbiota can influence the production of mood-regulating neurotransmitters like serotonin and dopamine. Moreover, the gut microbiota can also modulate the body’s stress response, which is often dysregulated in people with mood disorders.
Understanding the intricate relationship between gut health and mood disorders could open up new avenues for the prevention and treatment of these disorders. This article aims to delve into the science behind the gut-brain axis, explore how gut health can influence mood disorders, and discuss the potential of probiotics and dietary interventions in improving gut health and, consequently, mental health.
Table of contents
- Introduction: The Gut-Brain Connection
- The Science Behind the Gut-Brain Axis
- Gut Health and Depression
- Gut Health and Anxiety
- Probiotics and Mood Disorders
- Diet, Gut Health, and Mood Disorders
- Gut Health and Mood Disorders: The Role of Inflammation
- Improving Gut Health to Improve Mood Disorders
- Future Research on Gut Health and Mood Disorders
- Common Questions and Answers
The Science Behind the Gut-Brain Axis
Our bodies are intricate systems, where various parts do not work in isolation but are interconnected. One such fascinating connection is the gut-brain axis, a bidirectional communication system between our digestive tract and the brain. This system involves direct and indirect pathways between cognitive and emotional centers in the brain with peripheral intestinal functions. The vagus nerve is the main route of this communication superhighway, transmitting information from the gut to the brain.
But what’s truly intriguing is the role of the gut microbiome in this axis. The gut microbiome, a community of trillions of bacteria and other microbes living in our intestines, has a significant impact on the gut-brain axis. These microbes help digest our food, fight off harmful bacteria, and even produce various neurotransmitters. Neurotransmitters are chemical messengers that transmit signals throughout the body and have a significant impact on our mood and overall mental health.
For instance, about 90% of serotonin, commonly known as the ‘happy hormone’ for its role in regulating mood, is produced in the gut. Imbalances in the gut microbiome, often referred to as gut dysbiosis, can disrupt the production of serotonin and other neurotransmitters, potentially contributing to mood disorders.
Research has also found that gut bacteria produce other neuroactive substances, including gamma-aminobutyric acid (GABA), which has a calming effect on the body, and dopamine, which is involved in reward and pleasure systems. Changes in the levels of these substances can significantly affect our mood and mental health.
Furthermore, gut bacteria can stimulate the immune system, leading to the production of inflammation-causing chemicals known as cytokines. These cytokines can affect brain function and lead to mood disorders. This underlines the importance of a healthy gut microbiome not just for physical health, but mental health as well.
The gut-brain axis and the role of the gut microbiome in mental health is a rapidly growing field of research. It presents a paradigm shift in our understanding of mental health, suggesting that perhaps we should be paying as much attention to our gut health as we do to our brain health when it comes to managing and preventing mood disorders.
Gut Health and Depression
The link between gut health and mood disorders, such as depression, has gained significant attention in recent years. Emerging research suggests that the state of our gut can have a profound impact on our mental well-being. Let’s delve into the fascinating connection between gut health and depression.
The Science Behind the Gut-Brain Axis
Our gut and brain communicate through a bidirectional pathway known as the gut-brain axis. This intricate network involves the central nervous system, the enteric nervous system (which controls the digestive system), and the gut microbiota.
Gut Health and Depression
Studies have shown a strong association between gut health and depression. Individuals with depression often exhibit imbalances in their gut microbiota, with lower levels of beneficial bacteria and an overgrowth of harmful microbes.
Furthermore, research has found that those with depression have increased intestinal permeability, commonly referred to as “leaky gut.” This condition allows toxins and bacteria to leak into the bloodstream, triggering inflammation and potentially affecting brain function and mood regulation.
Gut Health and Anxiety
Anxiety disorders are closely linked to depression, and similar gut-brain interactions may be at play. Imbalances in gut bacteria and increased intestinal permeability have been observed in individuals with anxiety disorders.
Probiotics and Mood Disorders
Probiotics, which are beneficial bacteria, have shown promise in improving mood disorders. Certain strains, such as Lactobacillus and Bifidobacterium, have been found to reduce symptoms of depression and anxiety.
These probiotics work by restoring the balance of gut bacteria, reducing inflammation, and influencing neurotransmitter production. However, it’s important to note that the effects of probiotics can vary between individuals, and further research is needed to determine optimal dosages and specific strains for different mood disorders.
Diet, Gut Health, and Mood Disorders
Our diet plays a crucial role in maintaining a healthy gut and, consequently, promoting good mental health. A diet high in processed foods, sugar, and unhealthy fats can negatively impact the gut microbiota and increase the risk of mood disorders.
On the other hand, a diet rich in fruits, vegetables, whole grains, and lean proteins provides the necessary nutrients for a diverse and thriving gut microbiome. This type of diet, commonly referred to as the Mediterranean diet, has been associated with a lower risk of depression and improved mental well-being.
Gut Health and Mood Disorders: The Role of Inflammation
Inflammation is a key factor in the gut-brain connection. Chronic inflammation in the gut can lead to the release of inflammatory molecules that can affect brain function and contribute to the development of mood disorders.
Various factors, including an unhealthy diet, stress, lack of exercise, and environmental toxins, can trigger inflammation in the gut. By addressing these factors and promoting a healthy gut environment, it may be possible to reduce inflammation and alleviate symptoms of depression and anxiety.
Improving Gut Health to Improve Mood Disorders
There are several strategies to improve gut health and potentially alleviate symptoms of mood disorders:
- Include probiotic-rich foods, such as yogurt, sauerkraut, and kefir, in your diet.
- Consider taking a high-quality probiotic supplement, under the guidance of a healthcare professional.
- Eat a balanced diet with plenty of fiber, fruits, vegetables, and whole grains.
- Reduce the consumption of processed foods, sugar, and unhealthy fats.
- Manage stress through techniques like meditation, exercise, and relaxation exercises.
- Get regular exercise, as it has been shown to positively impact gut health and mood.
Future Research on Gut Health and Mood Disorders
While the connection between gut health and mood disorders is a promising area of research, there is still much to learn. Future studies will likely focus on identifying specific bacterial strains that have the most significant impact on mental health, developing personalized probiotics, and exploring the potential of gut-targeted therapies for mood disorders.
Common Questions and Answers
Q: Can improving gut health cure depression?
A: While improving gut health can potentially alleviate symptoms of depression, it is not a guaranteed cure. Depression is a complex condition with various contributing factors, and a holistic approach that includes therapy, medication, and lifestyle changes may be necessary.
Q: Are there any side effects of taking probiotics for mood disorders?
A: Probiotics are generally considered safe for most individuals. However, some people may experience mild digestive symptoms, such as bloating or gas, when first starting probiotic supplementation. If you have any concerns, it’s best to consult with a healthcare professional.
Q: Can gut health affect other mental health conditions?
A: Yes, research suggests that gut health may play a role in other mental health conditions, including bipolar disorder and schizophrenia. However, more studies are needed to fully understand these connections.
Q: How long does it take to see improvements in mood by improving gut health?
A: The timeline for seeing improvements in mood by improving gut health can vary. Some individuals may notice changes within a few weeks, while others may require several months of consistent lifestyle changes. It’s important to be patient and work closely with a healthcare professional.
Exploring the link between gut health and mood disorders offers promising insights into the potential for holistic approaches to mental well-being. By understanding and nurturing our gut microbiome, we may unlock new avenues for improving mental health and overall quality of life.
Gut Health and Anxiety
The gut-brain connection is a fascinating area of research that is shedding new light on the link between gut health and mood disorders. While much of the focus has been on the connection between gut health and depression, recent studies have also explored the relationship between gut health and anxiety.
Anxiety disorders are among the most common mental health conditions, affecting millions of people worldwide. Symptoms can range from mild to severe and can significantly impact a person’s quality of life. Understanding the underlying causes of anxiety and exploring potential treatments is crucial for improving outcomes for those affected.
Research has shown that there is a bidirectional communication between the gut and the brain, known as the gut-brain axis. This communication occurs through various pathways, including the nervous system, immune system, and endocrine system. The gut is home to trillions of bacteria, collectively known as the gut microbiota, which play a crucial role in maintaining gut health and influencing overall well-being.
Studies have found that individuals with anxiety disorders often have alterations in their gut microbiota composition compared to those without anxiety. These alterations can lead to increased inflammation in the gut, which can then affect the brain and contribute to the development or exacerbation of anxiety symptoms.
In addition to the gut microbiota, the gut lining also plays a vital role in maintaining gut health. When the gut lining becomes compromised, it can lead to a condition known as leaky gut syndrome. This condition allows toxins and bacteria to leak into the bloodstream, triggering an immune response and potentially leading to inflammation in the body, including the brain.
Emerging research suggests that improving gut health through various interventions, such as dietary changes and probiotic supplementation, may help alleviate anxiety symptoms. Probiotics, which are beneficial bacteria, have been shown to have a positive impact on gut health by restoring the balance of the gut microbiota and reducing inflammation.
Furthermore, certain dietary factors have been associated with an increased risk of anxiety disorders. A diet high in processed foods, sugar, and unhealthy fats can negatively impact gut health and contribute to inflammation. On the other hand, a diet rich in fruits, vegetables, whole grains, and lean proteins can support a healthy gut and potentially reduce anxiety symptoms.
It is important to note that while improving gut health may be beneficial for individuals with anxiety, it is not a standalone treatment. Anxiety disorders are complex conditions that often require a multidimensional approach, including therapy, medication, and lifestyle modifications.
Future research in this field aims to further elucidate the mechanisms underlying the gut-brain connection and explore additional interventions that may help improve gut health and alleviate anxiety symptoms. Understanding the link between gut health and anxiety opens up new avenues for potential treatment options and offers hope for individuals struggling with anxiety disorders.
Probiotics and Mood Disorders
Probiotics, the beneficial bacteria that reside in our gut, have gained significant attention in recent years for their potential role in improving gut health and overall well-being. Research has shown that these live microorganisms can have a positive impact on mood disorders such as depression and anxiety.
The gut microbiota, which consists of trillions of microorganisms, plays a crucial role in maintaining the health of our digestive system and influencing various aspects of our physical and mental health. The gut-brain axis, a bidirectional communication pathway between the gut and the brain, allows for constant communication and interaction between these two systems.
Studies have found that certain strains of probiotics can help regulate neurotransmitters in the brain, such as serotonin, dopamine, and gamma-aminobutyric acid (GABA), which are known to play a role in mood regulation. By modulating these neurotransmitters, probiotics may help alleviate symptoms of mood disorders.
One study published in the journal Psychiatry Research found that individuals who consumed a probiotic blend containing Lactobacillus acidophilus, Lactobacillus casei, and Bifidobacterium bifidum experienced significant improvements in their depression and anxiety symptoms compared to those who received a placebo.
Another study published in the journal Gut Microbes investigated the effects of a specific strain of probiotic called Lactobacillus rhamnosus on anxiety and stress. The results showed that individuals who consumed this probiotic had reduced anxiety and lower levels of the stress hormone cortisol.
While the exact mechanisms by which probiotics exert their effects on mood disorders are not yet fully understood, researchers believe that they may influence the production of neurotransmitters, reduce inflammation in the gut, and enhance the integrity of the intestinal barrier.
It’s important to note that not all probiotics are created equal, and different strains may have varying effects on mood disorders. Therefore, it is recommended to consult with a healthcare professional or a registered dietitian who can guide you in choosing the right probiotic supplement or food source.
In addition to taking probiotics, it is also essential to support a healthy gut microbiota through a balanced diet rich in fiber, fruits, vegetables, and fermented foods. These foods provide the necessary nutrients for the growth and maintenance of beneficial gut bacteria.
Furthermore, reducing stress levels, getting regular exercise, and prioritizing sleep can also contribute to a healthy gut and overall well-being.
While probiotics show promise in improving mood disorders, more research is needed to fully understand their efficacy, optimal dosage, and long-term effects. Ongoing studies are exploring the potential of personalized probiotic therapies tailored to an individual’s specific gut microbiota composition.
In conclusion, the link between gut health and mood disorders is a fascinating area of research, and probiotics offer a potential avenue for improving symptoms of depression and anxiety. Incorporating probiotics into a comprehensive approach that includes a healthy diet and lifestyle habits may contribute to better gut health and overall mental well-being.
Diet, Gut Health, and Mood Disorders
The relationship between diet, gut health, and mood disorders is a complex and fascinating area of research. It is becoming increasingly clear that what we eat can have a significant impact on our mental well-being. Let’s explore how our diet affects our gut health and, in turn, influences mood disorders such as depression and anxiety.
Our gut is home to trillions of microorganisms, collectively known as the gut microbiota. These microorganisms play a crucial role in maintaining the health of our digestive system and have far-reaching effects on our overall well-being, including our mental health.
Research has shown that a diet rich in fruits, vegetables, whole grains, and lean proteins can promote a diverse and healthy gut microbiota. On the other hand, a diet high in processed foods, sugar, and unhealthy fats can disrupt the balance of gut bacteria and contribute to inflammation in the body.
Several studies have found a correlation between a poor diet and an increased risk of mood disorders. For example, a diet high in refined sugars and saturated fats has been linked to a higher prevalence of depression. These types of foods can lead to inflammation in the body, which can negatively impact brain function and contribute to depressive symptoms.
Conversely, a diet rich in nutrients and beneficial compounds can support a healthy gut microbiota and improve mood. Certain foods, such as fatty fish rich in omega-3 fatty acids, have been shown to have anti-inflammatory effects and may help reduce symptoms of depression.
Additionally, probiotics, which are beneficial bacteria found in certain foods or supplements, have been studied for their potential to improve mood disorders. Probiotics can help restore the balance of gut bacteria and reduce inflammation, which may have a positive impact on mental health.
It’s important to note that while diet can play a significant role in gut health and mood disorders, it is not a standalone treatment. It should be used as part of a comprehensive approach that includes therapy, medication (if necessary), and other lifestyle interventions.
If you are experiencing symptoms of a mood disorder, it is essential to consult with a healthcare professional who can provide personalized advice and guidance. They can help you develop a treatment plan that takes into account your specific needs and circumstances.
In conclusion, the link between diet, gut health, and mood disorders is an area of growing interest in the field of mental health. Adopting a healthy diet that supports gut health, including a variety of fruits, vegetables, whole grains, and lean proteins, may have a positive impact on mood disorders. However, it is crucial to approach dietary changes as part of a comprehensive treatment plan under the guidance of a healthcare professional.
Gut Health and Mood Disorders: The Role of Inflammation
The role of inflammation in gut health and mood disorders is a topic of growing interest among researchers and healthcare professionals. In recent years, studies have shown a strong connection between inflammation in the gut and the development and progression of mood disorders such as depression and anxiety.
When the gut becomes inflamed, it can disrupt the delicate balance of neurotransmitters in the brain, leading to changes in mood, behavior, and cognition. The gut is home to trillions of bacteria, collectively known as the gut microbiota, which play a crucial role in maintaining gut health and overall well-being.
Imbalances in the gut microbiota, known as dysbiosis, can trigger an immune response and increase the production of pro-inflammatory cytokines. These cytokines can then travel to the brain and affect the functioning of neurotransmitters, such as serotonin, dopamine, and GABA, which are closely linked to mood regulation.
Research has shown that individuals with mood disorders often have higher levels of inflammatory markers in their blood and cerebrospinal fluid. Additionally, studies using animal models have demonstrated that inducing inflammation in the gut can lead to depressive-like behaviors.
Furthermore, chronic inflammation in the gut can impair the integrity of the intestinal barrier, also known as “leaky gut.” This allows toxins and bacteria to leak into the bloodstream, triggering an immune response and further exacerbating inflammation. The inflammatory response can then perpetuate a cycle of gut dysfunction and mood disorders.
It is important to note that while inflammation in the gut can contribute to the development of mood disorders, it is not the sole cause. Mood disorders are complex conditions influenced by a combination of genetic, environmental, and lifestyle factors. However, addressing gut health and reducing inflammation can be a valuable approach in managing and preventing mood disorders.
Various strategies can be employed to reduce inflammation and promote gut health. These include adopting a healthy diet rich in fiber, antioxidants, and omega-3 fatty acids, which can help nourish the gut microbiota and reduce inflammation. Regular exercise, stress management techniques, and adequate sleep also play a crucial role in maintaining a healthy gut and managing mood disorders.
Additionally, probiotics, which are beneficial bacteria that can restore the balance of the gut microbiota, have shown promising results in reducing inflammation and improving mood. Certain strains of probiotics, such as Lactobacillus and Bifidobacterium, have been found to have anti-inflammatory properties and can positively influence neurotransmitter activity.
While the link between gut health, inflammation, and mood disorders is still being explored, the emerging research suggests that addressing gut health can have a profound impact on mental well-being. By understanding and nurturing the gut-brain connection, we can potentially unlock new avenues for the prevention and treatment of mood disorders.
Improving Gut Health to Improve Mood Disorders
The link between gut health and mood disorders has sparked interest in finding ways to improve gut health as a means to alleviate symptoms of depression, anxiety, and other mood disorders. While research is still ongoing, there are several strategies that individuals can incorporate into their lifestyle to promote a healthy gut and potentially improve their mood.
1. Eat a Balanced Diet: A diet rich in whole foods, including fruits, vegetables, whole grains, lean proteins, and healthy fats, can support a diverse and healthy gut microbiome. Avoiding processed foods, excessive sugar, and artificial additives is also important for maintaining gut health.
2. Consume Probiotics: Probiotics are beneficial bacteria that can help restore and maintain a healthy balance of gut bacteria. They can be found in fermented foods such as yogurt, kefir, sauerkraut, and kimchi. Additionally, probiotic supplements are available over-the-counter.
3. Increase Fiber Intake: Fiber acts as a prebiotic, providing nourishment for the beneficial bacteria in the gut. Consuming a variety of fiber-rich foods such as fruits, vegetables, whole grains, and legumes can support a healthy gut and improve overall digestion.
4. Manage Stress: Chronic stress can negatively impact the gut microbiome and contribute to mood disorders. Engaging in stress-reducing activities such as exercise, meditation, deep breathing exercises, and spending time in nature can help improve gut health and promote emotional well-being.
5. Stay Hydrated: Drinking enough water is essential for maintaining a healthy gut. It helps in digestion, absorption of nutrients, and elimination of waste products. Aim to drink at least 8 glasses of water per day.
6. Get Adequate Sleep: Poor sleep quality and duration can disrupt the gut microbiome and contribute to mood disorders. Prioritize getting enough sleep by establishing a regular sleep schedule, creating a relaxing bedtime routine, and ensuring a comfortable sleep environment.
7. Limit Alcohol and Caffeine: Excessive alcohol consumption and high caffeine intake can disrupt the gut microbiome and worsen symptoms of mood disorders. Moderation is key when it comes to alcohol and caffeine consumption.
8. Consider Supplements: Certain supplements, such as omega-3 fatty acids, vitamin D, and magnesium, have been shown to support gut health and improve mood. However, it is important to consult with a healthcare professional before starting any new supplements.
It is important to note that improving gut health alone may not be a standalone treatment for mood disorders. It is recommended to work with a healthcare professional to develop a comprehensive treatment plan that may include therapy, medication, and lifestyle changes.
By incorporating these strategies into your daily routine, you can support a healthy gut and potentially improve mood disorders. However, it is always important to consult with a healthcare professional for personalized advice and guidance.
Future Research on Gut Health and Mood Disorders
As researchers continue to delve into the fascinating world of gut health and its connection to mood disorders, there are still many unanswered questions and areas that require further investigation. Future research in this field holds great promise for understanding the intricacies of the gut-brain axis and potentially developing new treatment approaches for mood disorders.
One area of future research is focused on identifying specific gut bacteria that play a role in mood regulation. While studies have shown a correlation between gut dysbiosis and mood disorders, the exact mechanisms underlying this connection remain unclear. By pinpointing the specific bacteria involved, researchers can gain a better understanding of how they influence mood and develop targeted interventions.
Another avenue for future research is exploring the impact of gut health on different types of mood disorders. While there is evidence linking gut health to depression and anxiety, it is important to investigate whether similar connections exist for other mood disorders, such as bipolar disorder or post-traumatic stress disorder. Understanding these relationships can help tailor treatment approaches to specific disorders.
Additionally, researchers are interested in determining the optimal interventions for improving gut health and alleviating mood disorders. While probiotics have shown promise in some studies, there is still a need for more robust clinical trials to establish their efficacy and identify the most effective strains and dosages. Furthermore, exploring the potential benefits of prebiotics, dietary interventions, and other gut health interventions can provide valuable insights into improving mood disorders.
The role of inflammation in gut health and mood disorders is another area that requires further investigation. Inflammation has been implicated in both gut dysbiosis and mood disorders, but the exact relationship between the two remains unclear. Future research can help elucidate the role of inflammation in the gut-brain axis and identify potential targets for intervention.
Longitudinal studies are also needed to understand the long-term effects of improving gut health on mood disorders. While some studies have shown short-term improvements in mood symptoms with interventions targeting gut health, it is important to assess the sustainability of these effects over time. Longitudinal studies can provide valuable information about the long-term benefits and potential relapse rates.
Lastly, future research should aim to identify the potential interactions between gut health and other factors known to influence mood disorders, such as genetics, stress, and lifestyle factors. Understanding these complex interactions can help develop a more comprehensive understanding of the gut-brain axis and inform personalized treatment approaches.
In conclusion, the field of gut health and mood disorders is still in its early stages, but the potential for future research is vast. By further exploring the gut-brain axis, identifying specific bacteria involved, investigating different mood disorders, optimizing interventions, understanding the role of inflammation, conducting longitudinal studies, and exploring interactions with other factors, researchers can contribute to a deeper understanding of this fascinating connection and pave the way for new and improved treatments for mood disorders.
Common Questions and Answers
Common Questions and Answers
Q: Can gut health really affect mood disorders?
A: Yes, research has shown a strong connection between gut health and mood disorders. The gut is often referred to as the “second brain” due to the intricate network of neurons lining the digestive system, known as the enteric nervous system. This system communicates bidirectionally with the central nervous system, influencing mood, emotions, and cognitive function.
Q: How does gut health influence depression?
A: Imbalances in the gut microbiota, the community of microorganisms living in the digestive tract, have been linked to depression. The gut microbiota produces neurotransmitters such as serotonin, which plays a key role in regulating mood. An unhealthy gut can lead to decreased serotonin production, potentially contributing to the development of depression.
Q: What about anxiety?
A: Similar to depression, anxiety disorders have also been associated with disruptions in gut health. Studies have shown that individuals with anxiety often have an altered gut microbiota composition compared to those without anxiety. By improving gut health, it may be possible to alleviate symptoms of anxiety.
Q: Can probiotics help with mood disorders?
A: Probiotics, which are beneficial bacteria, have shown promise in improving gut health and potentially alleviating symptoms of mood disorders. Certain strains of probiotics have been found to positively influence neurotransmitter production, reduce inflammation, and enhance the gut barrier function. However, more research is needed to determine the specific strains and dosages that are most effective.
Q: Is diet important for gut health and mood disorders?
A: Absolutely. The food we consume plays a significant role in shaping our gut microbiota. A diet high in processed foods, sugar, and unhealthy fats can negatively impact gut health and contribute to mood disorders. On the other hand, a diet rich in fruits, vegetables, whole grains, and fermented foods can promote a diverse and healthy gut microbiota, potentially improving mood and mental well-being.
Q: What role does inflammation play in gut health and mood disorders?
A: Inflammation in the body can have detrimental effects on both gut health and mood. Chronic inflammation can disrupt the delicate balance of the gut microbiota, leading to increased permeability of the gut barrier and systemic inflammation. This inflammatory response can contribute to the development and exacerbation of mood disorders.
Q: How can I improve my gut health to help with mood disorders?
A: There are several steps you can take to improve gut health and potentially alleviate symptoms of mood disorders. These include incorporating probiotic-rich foods into your diet, reducing stress levels, getting regular exercise, avoiding processed foods and added sugars, and consuming a diverse range of fruits, vegetables, and whole grains.
Q: What does the future hold for research on gut health and mood disorders?
A: The field of gut-brain research is still relatively new, and there is much more to uncover. Future studies will likely focus on identifying specific bacterial strains that have therapeutic potential, developing personalized dietary and probiotic interventions, and further exploring the mechanisms behind the gut-brain connection. Exciting advancements are expected in the coming years.