Introduction to Osteoarthritis of the Hip
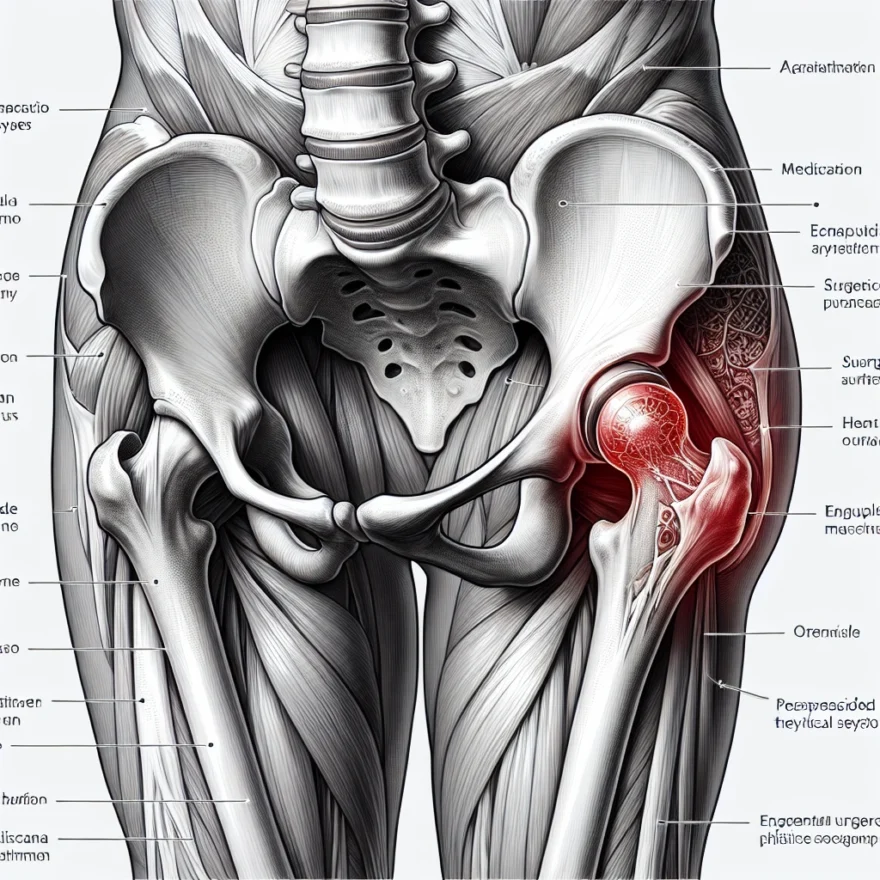
Osteoarthritis (OA) is a degenerative joint disease affecting millions of people worldwide. It is characterized by the gradual breakdown of cartilage, the protective tissue that cushions the ends of bones, allowing for smooth and pain-free joint movement. When cartilage deteriorates, bones can rub against each other, causing pain, stiffness, and reduced mobility. One of the most commonly affected joints is the hip, which plays a crucial role in supporting the body’s weight and allowing for a wide range of movements.
Hip osteoarthritis can significantly impact an individual’s quality of life, making everyday activities such as walking, climbing stairs, and even sitting for prolonged periods uncomfortable and challenging. As the condition progresses, it can lead to chronic pain and disability. Therefore, understanding the causes, symptoms, and available treatment options is essential for managing hip osteoarthritis effectively and maintaining an active, fulfilling life.
This comprehensive guide will provide an in-depth look at hip osteoarthritis, exploring its causes and risk factors, as well as how it is diagnosed. It will also discuss various non-surgical and surgical treatment options, the role of physical therapy and exercise, and the importance of lifestyle modifications in managing the condition. Additionally, the guide will cover assistive devices, alternative and complementary therapies, prevention strategies, and the emotional aspects of living with hip osteoarthritis. Finally, it will address frequently asked questions, emerging therapies, and resources and support available for patients navigating this complex medical condition.
Table of contents
- Introduction to Osteoarthritis of the Hip
- Causes and Risk Factors of Hip Osteoarthritis
- Symptoms and Diagnosis of Hip Osteoarthritis
- Non-Surgical Treatment Options for Hip Osteoarthritis
- Surgical Treatment Options for Hip Osteoarthritis
- Physical Therapy and Exercise for Hip Osteoarthritis
- Lifestyle Modifications for Managing Hip Osteoarthritis
- Assistive Devices for Hip Osteoarthritis
- Alternative and Complementary Therapies for Hip Osteoarthritis
- Preventing Hip Osteoarthritis: Tips for Healthy Joints
- When to Consider Hip Replacement Surgery
- Recovering from Hip Replacement Surgery
- Understanding the Risks and Complications of Hip Surgery
- The Role of Nutrition in Managing Hip Osteoarthritis
- The Impact of Weight Management on Hip Osteoarthritis
- Coping with the Emotional Aspects of Hip Osteoarthritis
- Frequently Asked Questions about Hip Osteoarthritis
- The Future of Hip Osteoarthritis Treatment: Emerging Therapies
- Resources and Support for Hip Osteoarthritis Patients
- Conclusion: Living Well with Hip Osteoarthritis
Causes and Risk Factors of Hip Osteoarthritis
Understanding the causes and risk factors of hip osteoarthritis is essential for both prevention and management of the condition. Osteoarthritis is a degenerative joint disease that affects the cartilage within the joints. In the case of hip osteoarthritis, the cartilage in the hip joint gradually wears away, leading to pain, stiffness, and reduced mobility. While the exact cause of hip osteoarthritis is not fully understood, several factors have been identified that may contribute to the development and progression of the condition.
Age: One of the most significant risk factors for hip osteoarthritis is age. As we grow older, our cartilage becomes more susceptible to wear and tear, making it more likely to break down over time. The majority of people diagnosed with hip osteoarthritis are over the age of 50.
Genetics: There is evidence to suggest that genetics may play a role in the development of hip osteoarthritis. If you have a family history of osteoarthritis, you may be at a higher risk of developing the condition yourself.
Gender: Women are more likely to develop hip osteoarthritis than men, particularly after the age of 50. This may be due to hormonal changes that occur during menopause, which can affect the health of the joints and cartilage.
Obesity: Carrying excess body weight places additional stress on the hip joints, which can accelerate the wear and tear of the cartilage. Maintaining a healthy weight is crucial for reducing the risk of hip osteoarthritis and managing the condition if it develops.
Joint injury or overuse: Injuries to the hip joint, such as fractures or dislocations, can increase the risk of developing osteoarthritis later in life. In addition, repetitive stress on the hip joint, often due to certain occupations or sports, can contribute to the breakdown of cartilage over time.
Other medical conditions: Certain medical conditions, such as rheumatoid arthritis, hip dysplasia, or avascular necrosis, can increase the risk of developing hip osteoarthritis by damaging the cartilage or affecting the joint’s blood supply.
It is important to note that not everyone with these risk factors will develop hip osteoarthritis, and some people may develop the condition without any known risk factors. However, being aware of these factors can help you take preventive measures to maintain the health of your hip joints and manage the condition if it develops.
Symptoms and Diagnosis of Hip Osteoarthritis
Osteoarthritis of the hip is a degenerative joint disease that affects millions of people worldwide. It is a chronic condition that causes the cartilage in the hip joint to wear down, resulting in bone-on-bone contact, inflammation, and pain. The symptoms of hip osteoarthritis can vary from person to person, but some common signs and symptoms include:
- Pain and stiffness in the hip joint, especially during movement
- Difficulty walking or standing for long periods of time
- Reduced range of motion in the hip joint
- Grinding or popping sensations in the hip joint
- Tenderness or swelling in the hip joint
If you are experiencing any of these symptoms, it is important to seek medical attention from a healthcare professional. Your doctor will perform a physical exam and may order imaging tests, such as X-rays or an MRI, to confirm a diagnosis of hip osteoarthritis.
During the physical exam, your doctor will assess your hip joint for signs of tenderness, swelling, and range of motion. They may also ask you to perform certain movements to assess the function of your hip joint. Imaging tests can provide a more detailed look at the hip joint and can help your doctor determine the extent of the damage to the joint.
It is important to note that hip osteoarthritis can sometimes be mistaken for other conditions, such as bursitis or tendinitis. This is why it is important to seek a proper diagnosis from a healthcare professional.
If you have been diagnosed with hip osteoarthritis, there are a variety of treatment options available to help manage your symptoms and improve your quality of life. These treatment options can include non-surgical interventions, such as physical therapy, exercise, and lifestyle modifications, as well as surgical interventions, such as hip replacement surgery.
It is important to work closely with your healthcare team to develop a treatment plan that is tailored to your individual needs and goals. With the right treatment and support, it is possible to live well with hip osteoarthritis and maintain an active and fulfilling lifestyle.
Non-Surgical Treatment Options for Hip Osteoarthritis
Managing osteoarthritis of the hip can be a challenging task, but there are several non-surgical treatment options available that can help alleviate symptoms and improve joint function. These treatment options are typically recommended as a first line of defense against hip osteoarthritis, and can be used in conjunction with other therapies for optimal results.
Physical Therapy
Physical therapy is a non-surgical treatment option that can help improve hip joint function and reduce pain associated with osteoarthritis. A physical therapist can work with you to develop an exercise program that is tailored to your specific needs and goals. This program may include strength training exercises to improve hip joint stability and flexibility exercises to improve range of motion.
Physical therapy can also include manual therapy techniques, such as massage and joint mobilization, to help reduce pain and improve joint function. Your physical therapist may also recommend other therapies, such as heat or ice therapy, to help alleviate pain and inflammation in the hip joint.
Medications
There are several medications that can be used to treat the symptoms of hip osteoarthritis. Over-the-counter pain relievers, such as acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs), can help reduce pain and inflammation in the hip joint. However, it is important to talk to your doctor before taking any new medications, as they can have side effects and may interact with other medications you are taking.
If over-the-counter medications are not effective in managing your symptoms, your doctor may prescribe stronger pain medications or corticosteroid injections. These medications can provide temporary relief from pain and inflammation in the hip joint.
Assistive Devices
Assistive devices, such as canes, crutches, and walkers, can help reduce pressure on the hip joint and improve mobility. These devices can be particularly helpful for individuals who are experiencing difficulty walking or standing due to hip osteoarthritis.
Additionally, your doctor may recommend the use of braces or shoe inserts to help improve hip joint alignment and reduce pain and discomfort.
Weight Management
Excess weight can put additional stress on the hip joint, exacerbating symptoms of osteoarthritis. Therefore, weight management is an important component of non-surgical treatment for hip osteoarthritis. Losing weight can help reduce pain and improve joint function, as well as decrease the risk of developing other health conditions associated with obesity.
Your doctor may recommend a combination of diet and exercise to help you achieve and maintain a healthy weight. A healthy diet should include plenty of fruits, vegetables, lean protein, and whole grains, while limiting processed foods and foods high in saturated and trans fats. Exercise can include low-impact activities, such as walking, swimming, and cycling, that are gentle on the hip joint and can help improve joint function and overall fitness.
Overall, non-surgical treatment options can be effective in managing the symptoms of hip osteoarthritis and improving joint function. However, it is important to work closely with your doctor to develop a treatment plan that is tailored to your specific needs and goals.
Surgical Treatment Options for Hip Osteoarthritis
When non-surgical treatments are not effective in managing hip osteoarthritis, surgical options may be considered. The decision to undergo surgery should be made in consultation with a healthcare provider and based on the individual’s specific needs and circumstances.
There are several surgical options available for hip osteoarthritis:
- Arthroscopy: This minimally invasive procedure involves inserting a small camera into the hip joint to visualize and repair any damage. It may be used to treat early-stage osteoarthritis or to diagnose and treat other hip conditions.
- Osteotomy: This procedure involves cutting and reshaping the bones around the hip joint to improve its alignment and reduce stress on the joint. It may be used in younger patients with early-stage osteoarthritis who are not yet candidates for hip replacement.
- Joint-preserving surgeries: These procedures aim to repair or replace damaged joint tissue while preserving the natural hip joint. They may be used in younger patients with early-stage osteoarthritis who wish to maintain their natural joint for as long as possible.
- Partial hip replacement: This procedure involves replacing only the damaged portion of the hip joint, leaving the healthy parts intact. It may be used in patients with localized osteoarthritis or other hip conditions that affect only a portion of the joint.
- Total hip replacement: This procedure involves replacing the entire hip joint with an artificial joint made of metal, plastic, or ceramic components. It is the most common surgical treatment for advanced hip osteoarthritis and can provide significant pain relief and improved function.
Each surgical option has its own risks and benefits, and the choice of procedure will depend on the individual’s age, health status, and the extent of their osteoarthritis. Recovery time and rehabilitation will also vary depending on the procedure performed.
It is important to discuss the potential risks and benefits of each surgical option with a healthcare provider, as well as any concerns or questions the individual may have. With proper care and management, surgical treatment can provide significant relief and improve quality of life for individuals with hip osteoarthritis.
Physical Therapy and Exercise for Hip Osteoarthritis
Physical therapy and exercise are important components of managing hip osteoarthritis. They help to improve joint mobility, reduce pain, and increase strength and flexibility. A physical therapist can work with you to develop an exercise program that is tailored to your individual needs.
The first step in physical therapy is to assess your current level of function and identify any areas of weakness or limitation. This may involve a series of tests and measurements to evaluate your range of motion, muscle strength, and joint stability. Based on this assessment, your physical therapist will develop a treatment plan that may include a combination of exercises, manual therapy, and other modalities.
One of the primary goals of physical therapy is to improve joint mobility. This may involve stretching exercises to increase flexibility and range of motion. Your physical therapist may also use manual therapy techniques, such as joint mobilization or soft tissue massage, to help improve joint mobility and reduce pain.
Strength training is also an important component of physical therapy for hip osteoarthritis. Strengthening exercises can help to improve muscle function and reduce stress on the joint. Your physical therapist may recommend exercises that target the muscles around the hip joint, such as the glutes, quadriceps, and hamstrings.
In addition to specific exercises, your physical therapist may also recommend cardiovascular exercise to improve overall fitness and reduce the risk of other health conditions. Low-impact activities such as walking, cycling, or swimming can be beneficial for people with hip osteoarthritis.
It is important to work closely with your physical therapist to ensure that your exercise program is safe and effective. Your therapist can provide guidance on proper form and technique, and can modify your program as needed based on your progress and any changes in your condition.
Overall, physical therapy and exercise can be effective in managing hip osteoarthritis and improving quality of life. By working with a physical therapist and following a tailored exercise program, you can reduce pain, improve joint mobility, and increase strength and flexibility.
Lifestyle Modifications for Managing Hip Osteoarthritis
Living with hip osteoarthritis can be challenging, but there are many lifestyle modifications that can help manage the symptoms and slow down the progression of the condition. These lifestyle changes can be simple, yet effective, and can improve your overall quality of life. Here are some lifestyle modifications that you can consider:
- Exercise regularly: Regular exercise can help strengthen the muscles around the hip joint, improve flexibility, and reduce pain. Low-impact exercises such as swimming, cycling, and walking are recommended for people with hip osteoarthritis. Consult with your doctor or physical therapist to determine the best exercise program for you.
- Manage your weight: Being overweight puts extra stress on your hip joint, which can worsen the symptoms of hip osteoarthritis. Losing weight can help reduce pain and slow down the progression of the condition. A balanced diet and regular exercise can help you maintain a healthy weight.
- Avoid high-impact activities: High-impact activities such as running and jumping can put a lot of stress on your hip joint and worsen the symptoms of hip osteoarthritis. Avoid these activities and opt for low-impact exercises instead.
- Use heat or cold therapy: Applying heat or cold to your hip joint can help reduce pain and stiffness. Use a heating pad or a warm towel to apply heat, or a cold pack or a bag of ice wrapped in a towel to apply cold therapy.
- Get enough rest: Rest is important for your body to heal and recover. Make sure you get enough sleep at night, and take breaks during the day to rest your hip joint.
- Use assistive devices: Assistive devices such as canes, crutches, and walkers can help reduce the pressure on your hip joint and improve your mobility. Consult with your doctor or physical therapist to determine which assistive device is best for you.
- Practice good posture: Good posture can help reduce the stress on your hip joint and improve your overall alignment. Make sure you sit and stand up straight, and avoid slouching or leaning to one side.
- Avoid prolonged sitting or standing: Prolonged sitting or standing can put a lot of pressure on your hip joint and worsen the symptoms of hip osteoarthritis. Take breaks and change positions frequently to reduce the pressure on your hip joint.
- Quit smoking: Smoking can worsen the symptoms of hip osteoarthritis and increase the risk of complications. Quitting smoking can help improve your overall health and reduce the progression of the condition.
By making these lifestyle modifications, you can manage the symptoms of hip osteoarthritis and improve your overall quality of life. Consult with your doctor or physical therapist to determine which lifestyle modifications are best for you.
Assistive Devices for Hip Osteoarthritis
Assistive devices can be helpful for people with hip osteoarthritis who experience pain and stiffness in their hip joint. These devices can help reduce the amount of stress on the joint and make it easier to perform daily activities. Here are some common types of assistive devices for hip osteoarthritis:
- Cane: A cane can help reduce the amount of weight that is placed on the hip joint while walking. It can also help improve balance and stability.
- Crutches: Crutches are another option for reducing weight on the hip joint while walking. They can be particularly helpful for people who have difficulty putting weight on one leg.
- Walker: A walker can provide more stability and support than a cane or crutches. It can also help distribute weight more evenly between both legs.
- Orthotics: Orthotic devices, such as shoe inserts or braces, can help improve the alignment of the hip joint and reduce stress on the joint.
- Grab bars: Grab bars can be installed in the bathroom or other areas of the home to provide support and stability when standing or sitting.
- Raised toilet seat: A raised toilet seat can make it easier to sit down and stand up from the toilet, reducing stress on the hip joint.
- Reacher: A reacher can help people with hip osteoarthritis avoid bending or reaching, which can be painful for the hip joint.
It’s important to note that assistive devices should be used in conjunction with other treatments for hip osteoarthritis, such as medication, physical therapy, and lifestyle modifications. A healthcare provider can help determine which assistive devices are most appropriate for an individual’s specific needs.
Alternative and Complementary Therapies for Hip Osteoarthritis
Osteoarthritis of the hip can be a debilitating condition that can greatly impact a person’s quality of life. While traditional treatments such as medication, physical therapy, and surgery can be effective, some people may also find relief through alternative and complementary therapies. These therapies can be used in conjunction with traditional treatments or on their own, depending on the individual’s needs and preferences.
Acupuncture
Acupuncture is an ancient Chinese practice that involves inserting thin needles into specific points on the body. It is believed to help stimulate the body’s natural healing processes, reduce inflammation, and relieve pain. Some studies have shown that acupuncture may be effective in reducing pain and improving function in people with hip osteoarthritis. However, more research is needed to fully understand its effectiveness.
Massage Therapy
Massage therapy involves the manipulation of soft tissues in the body, including muscles, tendons, and ligaments. It can help improve circulation, reduce muscle tension, and relieve pain. Some people with hip osteoarthritis may find that massage therapy helps to reduce their pain and improve their range of motion. However, it is important to work with a licensed massage therapist who has experience working with people with osteoarthritis.
Herbal Supplements
There are many herbal supplements that are believed to have anti-inflammatory and pain-relieving properties. Some of the most commonly used supplements for hip osteoarthritis include ginger, turmeric, and devil’s claw. While some people may find relief from these supplements, it is important to talk to a healthcare provider before taking any new supplements, as they can interact with other medications and have potential side effects.
Yoga and Tai Chi
Yoga and Tai Chi are both mind-body practices that can help improve flexibility, strength, and balance. They can also help reduce stress and improve overall well-being. Some studies have shown that these practices may be helpful in reducing pain and improving function in people with hip osteoarthritis. However, it is important to work with a qualified instructor who can modify the exercises to accommodate any physical limitations.
Chiropractic Care
Chiropractic care involves the manipulation of the spine and other joints in the body to help improve alignment and reduce pain. While there is limited research on the effectiveness of chiropractic care for hip osteoarthritis specifically, some people may find relief from this type of treatment. It is important to work with a licensed chiropractor who has experience working with people with osteoarthritis.
While alternative and complementary therapies can be helpful for some people with hip osteoarthritis, it is important to remember that they should not be used as a substitute for traditional medical care. It is always important to talk to a healthcare provider before starting any new treatments or supplements.
Preventing Hip Osteoarthritis: Tips for Healthy Joints
As the saying goes, prevention is better than cure. While it’s not always possible to prevent hip osteoarthritis, there are certain steps you can take to reduce your risk and keep your joints healthy. Here are some tips:
- Maintain a healthy weight: Excess weight puts extra stress on your joints, including your hips. Losing weight can help reduce your risk of developing hip osteoarthritis, as well as relieve symptoms if you already have the condition.
- Eat a balanced diet: A diet rich in fruits, vegetables, whole grains, and lean protein can help keep your joints healthy. Certain nutrients, such as vitamin C and omega-3 fatty acids, may also have anti-inflammatory effects that can help reduce joint pain and stiffness.
- Stay active: Regular exercise can help keep your joints flexible and strong. Low-impact activities like walking, swimming, and cycling are especially good for people with hip osteoarthritis, as they are less likely to cause joint pain and damage.
- Avoid repetitive motions: Doing the same movements over and over again can put stress on your joints and increase your risk of developing osteoarthritis. If you have a job or hobby that requires repetitive motions, take breaks often and switch up your movements when possible.
- Protect your joints: Wear appropriate protective gear when playing sports or engaging in other activities that put stress on your joints. Using proper form when lifting heavy objects can also help prevent joint injuries.
- Get regular check-ups: Seeing your doctor regularly can help catch joint problems early, before they become more serious. Your doctor can also give you advice on how to keep your joints healthy and prevent osteoarthritis.
While these tips can help reduce your risk of developing hip osteoarthritis, it’s important to remember that some factors, such as genetics and age, are beyond your control. If you do develop hip osteoarthritis, there are still many treatment options available to help manage your symptoms and improve your quality of life.
When to Consider Hip Replacement Surgery
When non-surgical treatments are no longer effective in managing hip osteoarthritis, hip replacement surgery may be considered. This is a major surgery that involves replacing the damaged hip joint with an artificial one.
Before deciding on surgery, it is important to discuss the risks and benefits with a healthcare provider. Factors such as age, overall health, and level of pain and disability will be taken into consideration when determining if surgery is the best option.
Some signs that it may be time to consider hip replacement surgery include:
- Severe pain that limits daily activities and interferes with sleep
- Stiffness or inability to move the hip joint
- Decreased range of motion in the hip joint
- Failure to respond to non-surgical treatments
- Progressive joint damage
It is important to note that hip replacement surgery is not a cure for hip osteoarthritis, but rather a way to manage pain and improve mobility. It is also a major surgery that carries risks such as infection, blood clots, and nerve damage.
Recovery time can vary, but typically involves a hospital stay of a few days and several weeks of physical therapy. It may take several months to fully recover and return to normal activities.
Overall, hip replacement surgery can be a life-changing procedure for those with severe hip osteoarthritis. It is important to carefully consider all options and work closely with a healthcare provider to determine if surgery is the right choice.
Recovering from Hip Replacement Surgery
Recovering from hip replacement surgery can be a long process, but it is a crucial part of ensuring a successful outcome. The recovery process will vary depending on the individual and the type of surgery performed, but there are some general guidelines that can help patients understand what to expect.
Immediately following surgery, patients will typically spend several days in the hospital. During this time, they will be closely monitored by medical staff and will begin physical therapy exercises to help them regain strength and mobility in the affected hip. Pain management will also be a top priority during this time, with medications and other treatments used to help manage discomfort.
After being discharged from the hospital, patients will continue their recovery at home. This will involve a combination of physical therapy exercises, pain management, and lifestyle modifications to help them avoid putting undue stress on the new hip joint. Patients may also need to use assistive devices such as crutches or walkers to help them get around while they recover.
It is important for patients to follow their doctor’s instructions closely during the recovery period. This may include attending physical therapy sessions, taking prescribed medications, and avoiding certain activities or movements that could disrupt the healing process. Patients should also be sure to get plenty of rest and eat a healthy, balanced diet to support their recovery.
Over time, patients will gradually begin to regain strength and mobility in the affected hip. However, it is important to remember that recovery is a slow process and that it may take several months before patients are able to resume normal activities. Patients should also be aware of the potential risks and complications associated with hip replacement surgery, and should contact their doctor immediately if they experience any unusual symptoms or complications during the recovery period.
Understanding the Risks and Complications of Hip Surgery
While hip replacement surgery is often a safe and effective treatment option for managing osteoarthritis of the hip, there are still risks and potential complications associated with the procedure. Some of the most common risks include infection, blood clots, and dislocation of the new hip joint.
Infection can occur after any surgery, and hip replacement surgery is no exception. To reduce the risk of infection, patients may be given antibiotics before and after the procedure, and the surgical team will take steps to maintain a sterile environment during the operation.
Another potential risk is the formation of blood clots in the legs, which can travel to the lungs and cause a pulmonary embolism. To prevent this, patients may be given blood thinners and encouraged to get up and move around as soon as possible after surgery.
Dislocation of the new hip joint is also a risk, particularly in the first few months after surgery. Patients will be given specific instructions on how to move and position their hip to minimize this risk, and may need to avoid certain activities or positions for a period of time.
Less common but still possible complications of hip replacement surgery include nerve damage, bone fractures, and implant failure. It’s important for patients to discuss these risks with their surgeon and understand the potential benefits and drawbacks of the procedure before making a decision.
Despite these risks, hip replacement surgery is generally considered safe and effective for most patients with severe hip osteoarthritis. By working closely with their healthcare team and following all pre- and post-operative instructions, patients can minimize their risk of complications and enjoy improved mobility and quality of life.
The Role of Nutrition in Managing Hip Osteoarthritis
Proper nutrition is an important factor in managing osteoarthritis of the hip. A healthy diet can help reduce inflammation, maintain a healthy weight, and provide the necessary nutrients to support joint health. Here are some dietary tips to consider:
- Include plenty of fruits and vegetables in your diet. These foods are rich in antioxidants and other nutrients that can help reduce inflammation and support joint health.
- Eat lean protein sources, such as fish, chicken, and beans. These foods provide the necessary building blocks for healthy muscles and joints.
- Choose whole grains over refined grains. Whole grains are rich in fiber, which can help regulate blood sugar levels and reduce inflammation.
- Limit your intake of processed and packaged foods, which are often high in salt, sugar, and unhealthy fats.
- Stay hydrated by drinking plenty of water throughout the day. Dehydration can make joint pain and stiffness worse.
- Consider taking supplements, such as omega-3 fatty acids, glucosamine, and chondroitin. These supplements have been shown to help reduce inflammation and support joint health.
It is also important to maintain a healthy weight when managing osteoarthritis of the hip. Excess weight puts additional stress on the joints, which can exacerbate symptoms and lead to further damage. Eating a healthy diet and engaging in regular exercise can help you achieve and maintain a healthy weight.
It is important to talk to your doctor or a registered dietitian before making any significant changes to your diet. They can help you develop a nutrition plan that meets your individual needs and supports your joint health.
The Impact of Weight Management on Hip Osteoarthritis
Weight management is an important aspect of managing osteoarthritis of the hip. Excess weight can put added stress on the hip joint, leading to increased pain and discomfort. Maintaining a healthy weight can help to reduce this stress and improve overall joint health.
There are a number of ways to manage weight when dealing with hip osteoarthritis. One of the most important is through diet. Eating a balanced diet that is rich in fruits, vegetables, and lean proteins can help to promote weight loss and improve overall health. Avoiding processed foods and sugary drinks can also be helpful in managing weight.
Exercise is another important component of weight management. Low-impact exercises such as swimming, cycling, and walking can help to burn calories and improve joint health without putting too much stress on the hip joint. Working with a physical therapist can be helpful in developing an exercise plan that is safe and effective for those with hip osteoarthritis.
In addition to diet and exercise, there are a number of other strategies that can be helpful in managing weight with hip osteoarthritis. These include getting enough sleep, managing stress, and avoiding smoking and excessive alcohol consumption. These lifestyle factors can all play a role in weight management and overall joint health.
Overall, weight management is an important aspect of managing hip osteoarthritis. By maintaining a healthy weight through diet, exercise, and lifestyle modifications, individuals with hip osteoarthritis can improve joint health and reduce pain and discomfort.
Coping with the Emotional Aspects of Hip Osteoarthritis
Living with hip osteoarthritis can be challenging not only physically but also emotionally. The pain, stiffness, and limitations in mobility can take a toll on your mental health and well-being. Coping with the emotional aspects of hip osteoarthritis is just as important as managing the physical symptoms.
Here are some tips for coping with the emotional aspects of hip osteoarthritis:
- Stay positive: It’s important to maintain a positive attitude and outlook. Focus on what you can do, not what you can’t. Celebrate small victories and progress.
- Seek support: Don’t be afraid to reach out to friends, family, or a support group for help. Talking to others who understand what you’re going through can be comforting and empowering.
- Stay active: Regular physical activity can help boost your mood and reduce stress. Choose low-impact activities that don’t aggravate your hip osteoarthritis, such as swimming or cycling.
- Practice relaxation techniques: Stress and anxiety can worsen pain and inflammation. Try relaxation techniques such as deep breathing, meditation, or yoga to help manage stress and promote relaxation.
- Stay informed: Educate yourself about hip osteoarthritis and treatment options. Knowing what to expect can help reduce anxiety and uncertainty.
- Don’t isolate yourself: It’s easy to withdraw from social activities when you’re in pain or feeling down. However, isolation can worsen depression and anxiety. Stay connected with loved ones and engage in social activities that you enjoy.
Remember, coping with the emotional aspects of hip osteoarthritis is just as important as managing the physical symptoms. By staying positive, seeking support, staying active, practicing relaxation techniques, staying informed, and not isolating yourself, you can improve your quality of life and overall well-being.
Frequently Asked Questions about Hip Osteoarthritis
What is osteoarthritis of the hip?
Osteoarthritis of the hip is a degenerative joint disease that affects the hip joint. It is a common condition that occurs when the cartilage in the joint wears down over time, causing pain, stiffness, and reduced mobility.
What are the causes of hip osteoarthritis?
The exact cause of hip osteoarthritis is not known, but it is believed to be caused by a combination of factors such as aging, genetics, joint injury, and obesity. These factors can lead to the breakdown of the cartilage in the hip joint, causing pain and stiffness.
What are the symptoms of hip osteoarthritis?
The symptoms of hip osteoarthritis include pain in the hip joint, stiffness, reduced range of motion, and difficulty walking. The pain may be worse after periods of inactivity or after physical activity. Some people may also experience a clicking or grinding sensation in the hip joint.
How is hip osteoarthritis diagnosed?
Diagnosis of hip osteoarthritis typically involves a physical examination, medical history, and imaging tests such as X-rays, MRI, or CT scans. A doctor may also perform a joint aspiration to rule out other conditions such as gout or rheumatoid arthritis.
What are the non-surgical treatment options for hip osteoarthritis?
Non-surgical treatment options for hip osteoarthritis include medications such as pain relievers and anti-inflammatory drugs, physical therapy, exercise, weight management, and assistive devices such as canes or walkers. In some cases, injections such as corticosteroids or hyaluronic acid may be recommended.
What are the surgical treatment options for hip osteoarthritis?
Surgical treatment options for hip osteoarthritis include hip replacement surgery, which involves replacing the damaged joint with an artificial joint. Other surgical options may include hip resurfacing or osteotomy. These procedures are typically recommended for people who have severe hip osteoarthritis and have not responded to non-surgical treatments.
What is the role of physical therapy and exercise in managing hip osteoarthritis?
Physical therapy and exercise can help improve range of motion, reduce pain, and increase strength and flexibility in the hip joint. Exercises may include low-impact activities such as swimming or cycling, as well as stretching and strengthening exercises.
What are some lifestyle modifications that can help manage hip osteoarthritis?
Lifestyle modifications that can help manage hip osteoarthritis include maintaining a healthy weight, avoiding activities that aggravate the hip joint, using assistive devices such as canes or walkers, and practicing good posture and body mechanics.
What are some alternative and complementary therapies for hip osteoarthritis?
Alternative and complementary therapies for hip osteoarthritis may include acupuncture, massage therapy, or chiropractic care. While these therapies may provide some relief from symptoms, they should be used in conjunction with traditional medical treatments.
What are some tips for preventing hip osteoarthritis?
Some tips for preventing hip osteoarthritis include maintaining a healthy weight, engaging in regular exercise, avoiding activities that may cause joint injury, and practicing good posture and body mechanics.
When should hip replacement surgery be considered?
Hip replacement surgery should be considered when non-surgical treatments have not provided adequate relief from symptoms, and the pain and stiffness in the hip joint are significantly impacting daily activities and quality of life.
What is the recovery process like after hip replacement surgery?
The recovery process after hip replacement surgery typically involves a period of rehabilitation and physical therapy. Most people are able to return to normal activities within a few months of surgery, but it may take up to a year to fully recover.
What are the risks and complications associated with hip replacement surgery?
The risks and complications associated with hip replacement surgery may include infection, blood clots, dislocation of the new joint, or nerve damage. However, these complications are rare and most people experience a successful outcome from the surgery.
How does nutrition impact hip osteoarthritis?
Nutrition can play a role in managing hip osteoarthritis, as a healthy diet can help maintain a healthy weight and reduce inflammation in the body. Foods that are rich in omega-3 fatty acids, such as fish and nuts, may be particularly beneficial.
How does weight management impact hip osteoarthritis?
Weight management can play a significant role in managing hip osteoarthritis, as excess weight can put added stress on the hip joint. Maintaining a healthy weight through a combination of diet and exercise can help reduce symptoms and slow the progression of the disease.
How can people cope with the emotional aspects of hip osteoarthritis?
Coping with the emotional aspects of hip osteoarthritis can be challenging, as the condition can impact daily activities and quality of life. Seeking support from family, friends, or a support group can be helpful, as can engaging in stress-reducing activities such as meditation or yoga.
What are some emerging therapies for hip osteoarthritis?
Emerging therapies for hip osteoarthritis may include stem cell therapy, platelet-rich plasma injections, or gene therapy. While these therapies are still in the early stages of development, they may hold promise for the future of hip osteoarthritis treatment.
Where can people find resources and support for hip osteoarthritis?
Resources and support for hip osteoarthritis may be available through local hospitals or medical centers, as well as through online support groups or advocacy organizations such as the Arthritis Foundation.
What is the outlook for people with hip osteoarthritis?
The outlook for people with hip osteoarthritis varies depending on the severity of the condition and the effectiveness of treatment. With proper management and treatment, most people with hip osteoarthritis are able to maintain an active lifestyle and manage their symptoms effectively.
The Future of Hip Osteoarthritis Treatment: Emerging Therapies
As medical research continues to advance, new therapies for hip osteoarthritis are being developed and tested. One promising emerging therapy is stem cell therapy. Stem cells are cells that have the ability to develop into various types of cells in the body. In stem cell therapy, stem cells are harvested from the patient’s own body (usually from bone marrow or fat tissue), processed and then injected into the affected joint. The stem cells then differentiate into cartilage cells, which can help to repair the damaged joint tissue.
Another emerging therapy for hip osteoarthritis is platelet-rich plasma (PRP) therapy. In PRP therapy, a sample of the patient’s blood is taken and processed to concentrate the platelets, which contain growth factors that can help to promote healing. The concentrated platelets are then injected into the affected joint.
Gene therapy is also being explored as a potential treatment for hip osteoarthritis. In gene therapy, genes are introduced into the body to help produce proteins that can repair damaged tissue. This therapy is still in the experimental stage, but early studies have shown promising results.
Finally, researchers are exploring the use of 3D printing technology to create custom implants for hip replacement surgery. These implants would be designed specifically for each patient’s unique anatomy, potentially reducing the risk of complications and improving outcomes.
Resources and Support for Hip Osteoarthritis Patients
Living with hip osteoarthritis can be challenging, but there are resources and support available to help you manage the condition and improve your quality of life. Here are some options to consider:
- Arthritis Foundation: The Arthritis Foundation is a nonprofit organization that provides education, advocacy, and support for people with arthritis. They offer resources specifically for those with hip osteoarthritis, including information on treatments, exercise programs, and local support groups.
- National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS): NIAMS is a government organization that funds research and provides information on a variety of musculoskeletal conditions, including osteoarthritis. Their website offers a wealth of information on hip osteoarthritis, including treatment options, self-care tips, and resources for finding clinical trials.
- Local support groups: Connecting with others who are also living with hip osteoarthritis can be a valuable source of support and information. Consider reaching out to local support groups or organizations, such as the Arthritis Foundation, to find groups in your area.
- Physical therapists: A physical therapist can help you develop an exercise program tailored to your specific needs and limitations. They can also provide guidance on managing pain and improving mobility.
- Occupational therapists: An occupational therapist can help you make modifications to your home or workplace to make daily activities easier and less painful. They can also provide guidance on using assistive devices, such as canes or walkers.
- Counselors or therapists: Coping with a chronic condition like hip osteoarthritis can be emotionally challenging. Consider seeing a counselor or therapist to help you manage stress, anxiety, or depression.
Remember, you don’t have to face hip osteoarthritis alone. There are many resources and support options available to help you manage the condition and live your best life.
Conclusion: Living Well with Hip Osteoarthritis
Living Well with Hip Osteoarthritis
Managing hip osteoarthritis can be challenging, but with the right approach, it is possible to live well with this condition. By understanding the causes, symptoms, and treatment options for hip osteoarthritis, you can take control of your health and improve your quality of life.
Non-surgical treatments such as medications, physical therapy, and lifestyle modifications can help relieve pain and improve mobility. These treatments can also help slow the progression of hip osteoarthritis and prevent further damage to the joint.
Surgical options such as hip replacement surgery can provide long-term relief for severe cases of hip osteoarthritis. However, it is important to understand the risks and potential complications of surgery before making a decision.
In addition to medical treatments, there are many things you can do to manage hip osteoarthritis on a daily basis. Maintaining a healthy weight, staying active, and using assistive devices such as canes or walkers can all help reduce pain and improve mobility.
It is also important to take care of your emotional well-being when living with hip osteoarthritis. Coping with chronic pain and limited mobility can be challenging, but seeking support from loved ones or a mental health professional can help.
By taking a proactive approach to managing hip osteoarthritis, you can continue to enjoy your favorite activities and maintain your independence. With the right tools and resources, you can live well with hip osteoarthritis and maintain a high quality of life.