Introduction to Myasthenia Gravis
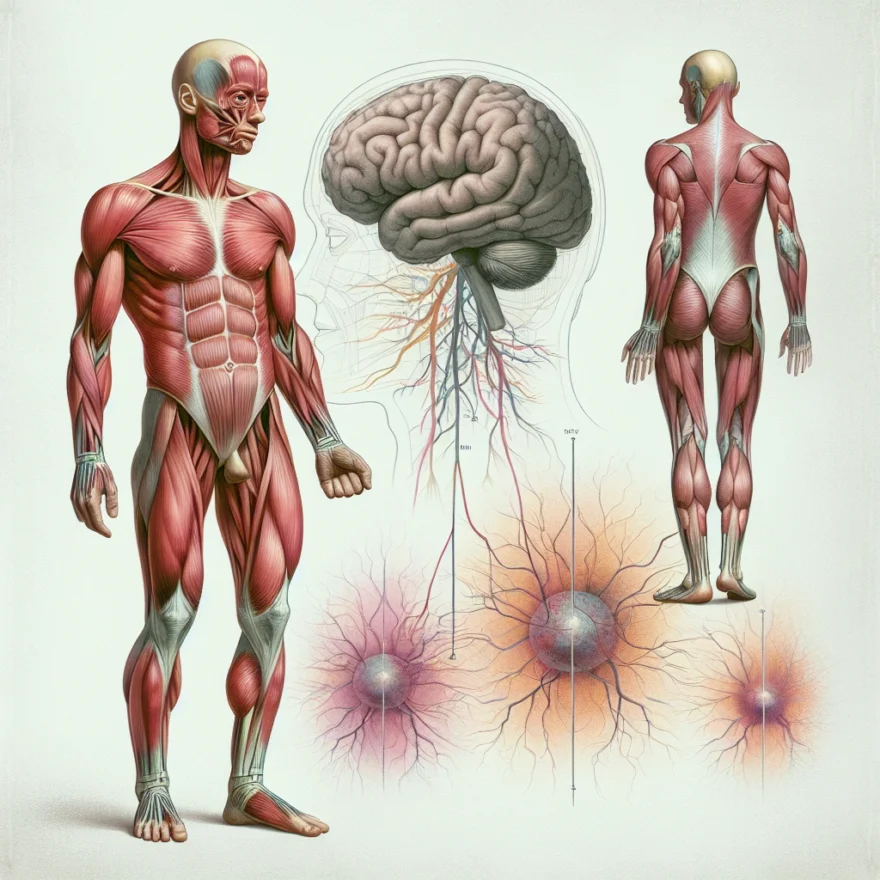
Myasthenia Gravis is a chronic autoimmune neuromuscular disease characterized by varying degrees of weakness in the skeletal muscles, which are responsible for movement. The name Myasthenia Gravis, which is Greek and Latin in origin, translates to “grave, or serious, muscle weakness.” This disorder affects the communication between nerves and muscles, leading to an inability of the muscles to contract properly and causing muscle weakness.
It is a relatively rare condition, affecting approximately 20 people in every 100,000 in the United States, according to the National Institute of Neurological Disorders and Stroke. The disease can occur at any age but is most common in women under 40 and men over 60. It is not directly inherited nor is it contagious. However, it can occur in more than one member of the same family.
Myasthenia Gravis is often associated with other autoimmune disorders, including thyroid disease, lupus, and rheumatoid arthritis. The onset of the disease can be sudden, and symptoms often are not immediately recognized as Myasthenia Gravis. The severity of the disease varies greatly among individuals, ranging from a localized form limited to eye muscles (ocular myasthenia), to a severe or generalized form in which many muscles – sometimes including those that control breathing – are affected.
Despite its name, with proper treatment, most individuals with Myasthenia Gravis can significantly improve their muscle weakness and lead normal or nearly normal lives. Many people with the condition have a normal life expectancy. However, untreated, the disease can lead to significant morbidity and mortality, particularly through respiratory failure. Therefore, early recognition and proper treatment are important.
Table of contents
- Introduction to Myasthenia Gravis
- Understanding the Neuromuscular Junction
- Causes of Myasthenia Gravis
- Symptoms of Myasthenia Gravis
- Diagnosis of Myasthenia Gravis
- Treatment Options for Myasthenia Gravis
- Living with Myasthenia Gravis
- Research and Future Directions in Myasthenia Gravis
- Common Questions and Answers about Myasthenia Gravis
Understanding the Neuromuscular Junction
To fully grasp the complexity of Myasthenia Gravis, it’s crucial to first comprehend the functionality of the neuromuscular junction. This is the point of contact between a nerve cell (neuron) and a muscle cell (myocyte). It’s a specialized synapse, a structure that allows a neuron to pass an electrical or chemical signal to another cell. In essence, it’s the communication bridge that facilitates the conversion of electrical signals from the brain into mechanical muscle action.
When a nerve impulse reaches the end of the neuron, it triggers the release of a neurotransmitter called acetylcholine. This chemical messenger travels across the tiny gap (synaptic cleft) between the nerve and muscle cell, binding to acetylcholine receptors on the muscle cell surface. This binding sparks a chain of events that ultimately leads to muscle contraction.
After the acetylcholine has done its job, an enzyme called acetylcholinesterase breaks it down, and the muscle cell relaxes until the next nerve impulse arrives. This intricate process happens countless times every second, allowing us to perform both voluntary movements like walking and involuntary actions like breathing.
In the case of Myasthenia Gravis, this communication system is disrupted. The body’s own immune system mistakenly targets and damages the acetylcholine receptors, leading to a reduction in the number of functional receptors. As a result, not enough acetylcholine can bind to the muscle cells, impairing their ability to contract and causing the characteristic muscle weakness seen in this disorder.
Causes of Myasthenia Gravis
Myasthenia Gravis is a neuromuscular disorder characterized by muscle weakness. The exact cause of this condition is not fully understood, but researchers believe that it is primarily an autoimmune disorder. In autoimmune diseases, the body’s immune system mistakenly attacks its own tissues.
In the case of Myasthenia Gravis, the immune system targets the neuromuscular junction, which is the point where nerve cells connect with the muscles they control. Normally, nerve cells release a chemical called acetylcholine, which binds to receptors on the muscle cells, causing them to contract. However, in individuals with Myasthenia Gravis, the immune system produces antibodies that block or destroy these receptors, leading to muscle weakness and fatigue.
While the exact trigger for the development of Myasthenia Gravis is unknown, several factors are believed to contribute to its onset:
- Genetics: There is evidence to suggest that certain genetic factors may increase the susceptibility to developing Myasthenia Gravis. However, it is important to note that having a family history of the condition does not guarantee its development.
- Thymus gland abnormalities: The thymus gland, which plays a role in the development of the immune system, is often abnormal in individuals with Myasthenia Gravis. It is believed that the presence of certain abnormal cells in the thymus gland may trigger an autoimmune response.
- Environmental factors: Some researchers believe that certain environmental factors, such as viral infections or exposure to certain medications, may play a role in the development of Myasthenia Gravis. However, more research is needed to fully understand the relationship between these factors and the condition.
It is important to note that while these factors may contribute to the development of Myasthenia Gravis, they do not guarantee its onset. The condition can still occur in individuals without any known risk factors.
Symptoms of Myasthenia Gravis
Myasthenia Gravis is a neuromuscular disorder that can cause muscle weakness and fatigue. The symptoms of this condition can vary from person to person, but they generally involve the muscles that control movement and breathing.
One of the most common symptoms of Myasthenia Gravis is muscle weakness, which typically worsens with activity and improves with rest. This weakness can affect various muscles in the body, including those in the face, neck, arms, and legs. Some individuals may experience difficulty with activities such as lifting objects, climbing stairs, or even holding their head up.
Another common symptom is fatigue, which can be both physical and mental. People with Myasthenia Gravis often report feeling tired easily, even after minimal exertion. This fatigue can impact daily activities and may require individuals to take frequent breaks or rest periods.
In addition to muscle weakness and fatigue, individuals with Myasthenia Gravis may also experience other symptoms such as:
- Drooping eyelids (ptosis)
- Double vision (diplopia)
- Difficulty speaking or swallowing
- Changes in facial expression
- Weakness in the muscles that control the respiratory system
- Difficulty chewing or controlling facial movements
These symptoms can vary in severity and may come and go, making the diagnosis of Myasthenia Gravis challenging. It is important to note that symptoms may worsen with physical or emotional stress, and can also be influenced by factors such as time of day or medication use.
If you are experiencing any of these symptoms, it is important to consult with a healthcare professional for a proper diagnosis. They will be able to evaluate your symptoms, perform necessary tests, and develop a treatment plan tailored to your specific needs.
Diagnosis of Myasthenia Gravis
Diagnosing Myasthenia Gravis can be a complex process, as its symptoms can vary widely and mimic other conditions. However, with the help of medical professionals and specialized tests, an accurate diagnosis can be made. Here are some of the key diagnostic methods used for Myasthenia Gravis:
Medical History and Physical Examination: The diagnosis of Myasthenia Gravis often begins with a thorough medical history and physical examination. The healthcare provider will ask about the patient’s symptoms, their progression, and any family history of the disorder. They will also perform a detailed physical examination, focusing on muscle weakness and any other neurological abnormalities.
Neurological Evaluation: A neurological evaluation is crucial in diagnosing Myasthenia Gravis. This evaluation may include tests to assess muscle strength, reflexes, and coordination. The healthcare provider may also look for specific signs, such as drooping eyelids or difficulty swallowing, which are common in Myasthenia Gravis.
Edrophonium Test: The edrophonium test is a commonly used diagnostic test for Myasthenia Gravis. During this test, a small dose of the medication edrophonium chloride is injected into the patient. If the patient has Myasthenia Gravis, there is a temporary improvement in muscle strength. This test helps to differentiate between Myasthenia Gravis and other conditions that may cause muscle weakness.
Electromyography (EMG): Electromyography is a test that measures the electrical activity of muscles. It can help determine if muscle weakness is caused by a problem with the nerves or the muscles themselves. In Myasthenia Gravis, the EMG may show characteristic patterns of muscle fatigue and weakness.
Blood Tests: Blood tests can be useful in diagnosing Myasthenia Gravis. These tests can detect the presence of specific antibodies, such as acetylcholine receptor antibodies (AChR) or muscle-specific kinase antibodies (MuSK), which are often found in individuals with Myasthenia Gravis. However, it’s important to note that not all individuals with Myasthenia Gravis have detectable antibodies.
Imaging Studies: In some cases, imaging studies such as a chest X-ray or computed tomography (CT) scan may be performed. These tests can help identify any abnormalities in the thymus gland, which is often associated with Myasthenia Gravis.
Repetitive Nerve Stimulation (RNS): Repetitive nerve stimulation is a test that measures how well the nerves are conducting impulses to the muscles. In Myasthenia Gravis, the RNS test may show a characteristic decrease in muscle response with repetitive stimulation.
It’s important to note that the diagnostic process may vary for each individual, and additional tests may be required to confirm a diagnosis of Myasthenia Gravis. Consulting with a healthcare professional who specializes in neuromuscular disorders is essential for an accurate diagnosis.
Treatment Options for Myasthenia Gravis
Myasthenia Gravis is a complex neuromuscular disorder that causes muscle weakness and fatigue. While there is no cure for this condition, there are various treatment options available to manage the symptoms and improve the quality of life for individuals with Myasthenia Gravis.
1. Medications:
One of the primary treatment approaches for Myasthenia Gravis is the use of medications. The most commonly prescribed medications for this condition include:
- Cholinesterase inhibitors: These medications help improve muscle strength and function by blocking the enzyme that breaks down acetylcholine, a neurotransmitter involved in muscle contractions.
- Immunosuppressants: These medications suppress the immune system to reduce the production of antibodies that attack the neuromuscular junction. Commonly prescribed immunosuppressants include corticosteroids, azathioprine, mycophenolate, and methotrexate.
- Monoclonal antibodies: In some cases, monoclonal antibodies like rituximab or eculizumab may be used to target specific immune cells and reduce the production of harmful antibodies.
2. Thymectomy:
A thymectomy is a surgical procedure that involves the removal of the thymus gland. The thymus gland is believed to play a role in the development of Myasthenia Gravis, and removing it can help improve symptoms and reduce the need for medications in some individuals.
3. Plasmapheresis:
Plasmapheresis, also known as plasma exchange, is a procedure that involves removing the plasma from the blood and replacing it with donor plasma or a plasma substitute. This technique helps remove the harmful antibodies from the bloodstream, providing temporary relief from Myasthenia Gravis symptoms.
4. Intravenous Immunoglobulin (IVIG) Therapy:
IVIG therapy involves receiving high doses of immunoglobulin through intravenous infusion. Immunoglobulins are proteins that help regulate the immune system and can temporarily improve muscle strength in individuals with Myasthenia Gravis.
5. Physical Therapy:
In addition to medical interventions, physical therapy plays a crucial role in managing Myasthenia Gravis. Physical therapists can design exercise programs to improve muscle strength, flexibility, and coordination, helping individuals with Myasthenia Gravis maintain their independence and functionality.
6. Lifestyle Modifications:
Adopting certain lifestyle modifications can also help individuals with Myasthenia Gravis manage their symptoms effectively. These may include:
- Conserving energy by taking regular breaks and pacing activities.
- Eating a well-balanced diet to maintain overall health and muscle function.
- Avoiding triggers that worsen symptoms, such as stress, extreme temperatures, and certain medications.
- Seeking support from friends, family, and support groups to cope with the emotional and psychological impact of the condition.
It is important for individuals with Myasthenia Gravis to work closely with their healthcare team to determine the most appropriate treatment plan for their specific needs. Treatment options may vary depending on the severity of symptoms, age, overall health, and individual preferences.
While there is ongoing research to find new and improved treatment options for Myasthenia Gravis, the current treatment approaches have shown significant success in managing the symptoms and improving the quality of life for individuals living with this condition.
Living with Myasthenia Gravis
Living with Myasthenia Gravis can be challenging, but with proper management and support, individuals with this condition can lead fulfilling lives. Here are some important aspects to consider:
1. Self-Care and Lifestyle Modifications
It is crucial for individuals with Myasthenia Gravis to prioritize self-care and make necessary lifestyle modifications. This includes getting enough rest and sleep to prevent fatigue, which can exacerbate muscle weakness. It is also important to maintain a healthy diet, exercise regularly, and manage stress levels. Additionally, avoiding triggers such as certain medications or infections that can worsen symptoms is essential.
2. Medication Adherence
Adhering to the prescribed medication regimen is vital in managing Myasthenia Gravis. Medications such as acetylcholinesterase inhibitors and immunosuppressants help improve muscle strength and reduce symptoms. It is important to take medications as directed by the healthcare provider and to communicate any concerns or side effects experienced.
3. Assistive Devices and Mobility Aids
Depending on the severity of muscle weakness, individuals with Myasthenia Gravis may benefit from using assistive devices and mobility aids. This can include walking aids like canes or walkers, or even motorized scooters for longer distances. These devices can help conserve energy and improve mobility, allowing individuals to maintain their independence.
4. Emotional Support and Mental Health
Living with a chronic condition like Myasthenia Gravis can take a toll on mental health. It is important for individuals to seek emotional support from friends, family, or support groups. Connecting with others who have similar experiences can provide a sense of understanding and empathy. Additionally, seeking therapy or counseling can help individuals cope with the emotional challenges associated with the condition.
5. Regular Follow-ups and Communication with Healthcare Providers
Regular follow-up appointments with healthcare providers, such as neurologists or rheumatologists, are crucial in managing Myasthenia Gravis. These appointments allow for monitoring of symptoms, adjustment of medications if necessary, and addressing any concerns or questions. Open and honest communication with healthcare providers is key to ensuring optimal management of the condition.
6. Planning and Preparation
Planning and preparation are essential for individuals with Myasthenia Gravis to navigate daily activities effectively. This can include organizing medication schedules, planning rest periods throughout the day, and making necessary accommodations in the workplace or school settings. Having a support system in place and communicating needs with employers or educational institutions can help facilitate a smooth and manageable routine.
By implementing these strategies and seeking appropriate support, individuals with Myasthenia Gravis can improve their quality of life and effectively manage their condition.
Research and Future Directions in Myasthenia Gravis
Research and Future Directions in Myasthenia Gravis
Myasthenia Gravis is a complex neuromuscular disorder that continues to be a subject of extensive research. Scientists and medical professionals are dedicated to understanding the underlying mechanisms of the disease and developing more effective treatments. Here are some of the exciting research areas and future directions in the field of Myasthenia Gravis:
1. Immunotherapy: One of the main focuses of research is developing new immunotherapies for Myasthenia Gravis. Current treatments aim to suppress the immune system, but researchers are investigating novel approaches to modulate the immune response more specifically. This includes exploring the potential of targeted therapies that can reduce the production of autoantibodies responsible for attacking the neuromuscular junction.
2. Genetic Studies: Understanding the genetic factors contributing to Myasthenia Gravis is another area of active research. Scientists are conducting large-scale genetic studies to identify specific genes associated with the disease. This knowledge can help in early diagnosis, predicting disease severity, and developing personalized treatment strategies.
3. Stem Cell Therapy: Stem cell therapy holds promise for the treatment of various diseases, including Myasthenia Gravis. Researchers are exploring the potential of using stem cells to repair and regenerate damaged muscle cells and restore normal neuromuscular function. Although still in the early stages, this approach shows great potential for future therapeutic interventions.
4. Novel Drug Development: Pharmaceutical companies and research institutions are actively working on developing new drugs specifically targeting the underlying mechanisms of Myasthenia Gravis. These drugs aim to improve muscle strength, reduce symptoms, and minimize side effects. Clinical trials are underway to evaluate the safety and efficacy of these potential treatments.
5. Improved Diagnostic Techniques: Researchers are continually striving to develop more accurate and efficient diagnostic techniques for Myasthenia Gravis. This includes the use of advanced imaging technologies, such as PET scans and MRI, to visualize the neuromuscular junction and assess its functionality. These advancements can lead to earlier and more precise diagnoses, allowing for timely intervention and management of the disease.
6. Patient Support and Education: In addition to scientific research, efforts are being made to enhance patient support and education programs for individuals living with Myasthenia Gravis. These initiatives aim to improve the quality of life for patients by providing them with resources, information, and a supportive community. Online forums, support groups, and educational materials play a crucial role in empowering patients and their families.
As research in Myasthenia Gravis progresses, it offers hope for better understanding, diagnosis, and treatment options for individuals affected by this debilitating condition. The collaboration between researchers, clinicians, and patients is vital in driving advancements and improving the lives of those living with Myasthenia Gravis.
Common Questions and Answers about Myasthenia Gravis
Common Questions and Answers about Myasthenia Gravis
Myasthenia Gravis (MG) is a complex neuromuscular disorder that can raise many questions for those affected by it. In this section, we aim to address some of the common questions and provide answers to help you better understand this condition.
1. What exactly is Myasthenia Gravis?
Myasthenia Gravis is a chronic autoimmune disorder that affects the muscles and the nerves that control them. It is characterized by muscle weakness and fatigue, which typically worsen with activity and improve with rest.
2. What causes Myasthenia Gravis?
The exact cause of Myasthenia Gravis is not fully understood, but it is believed to be an autoimmune condition, where the body’s immune system mistakenly attacks the neuromuscular junction. In some cases, it may be associated with thymus gland abnormalities or certain genetic factors.
3. What are the common symptoms of Myasthenia Gravis?
The most common symptom of Myasthenia Gravis is muscle weakness, which typically affects the muscles that control eye movements, facial expressions, chewing, swallowing, and speaking. Other symptoms may include drooping eyelids, double vision, difficulty breathing, and fatigue.
4. How is Myasthenia Gravis diagnosed?
Diagnosing Myasthenia Gravis involves a combination of medical history evaluation, physical examination, and various tests such as blood tests, nerve conduction studies, electromyography, and a special test called the edrophonium test. These tests help to confirm the presence of the condition and determine its severity.
5. What treatment options are available for Myasthenia Gravis?
Treatment for Myasthenia Gravis aims to manage symptoms, improve muscle strength, and prevent complications. This may include medications such as cholinesterase inhibitors and immunosuppressants, thymectomy (surgical removal of the thymus gland), plasmapheresis, and intravenous immunoglobulin (IVIG) therapy.
6. How can I live with Myasthenia Gravis?
Living with Myasthenia Gravis requires a multidisciplinary approach. It is important to work closely with healthcare professionals to develop a personalized treatment plan, manage symptoms, conserve energy, and make necessary lifestyle adjustments. Support groups and counseling can also provide emotional support and helpful tips for coping with the condition.
7. What is the current research and future direction in Myasthenia Gravis?
Ongoing research in Myasthenia Gravis aims to further understand the underlying mechanisms of the condition, develop more targeted therapies, and improve diagnostic techniques. Advances in immunology and genetics are providing new insights into potential treatment options and the possibility of personalized medicine for individuals with Myasthenia Gravis.
8. Can Myasthenia Gravis be cured?
As of now, there is no cure for Myasthenia Gravis. However, with proper management and treatment, most individuals with the condition can lead fulfilling lives. It is important to work closely with healthcare professionals to effectively control symptoms and minimize the impact of the condition on daily activities.
9. Can Myasthenia Gravis be passed on to children?
While Myasthenia Gravis is not directly inherited, certain genetic factors may increase the risk of developing the condition. It is recommended to consult with a genetic counselor if you have a family history of Myasthenia Gravis or if you are planning to have children.
10. Are there any lifestyle changes that can help manage Myasthenia Gravis?
Yes, certain lifestyle changes can help manage Myasthenia Gravis. These may include pacing activities to conserve energy, eating a balanced diet, getting regular exercise (as recommended by your healthcare professional), managing stress levels, and avoiding triggers that worsen symptoms.