Understanding Tuberous Sclerosis
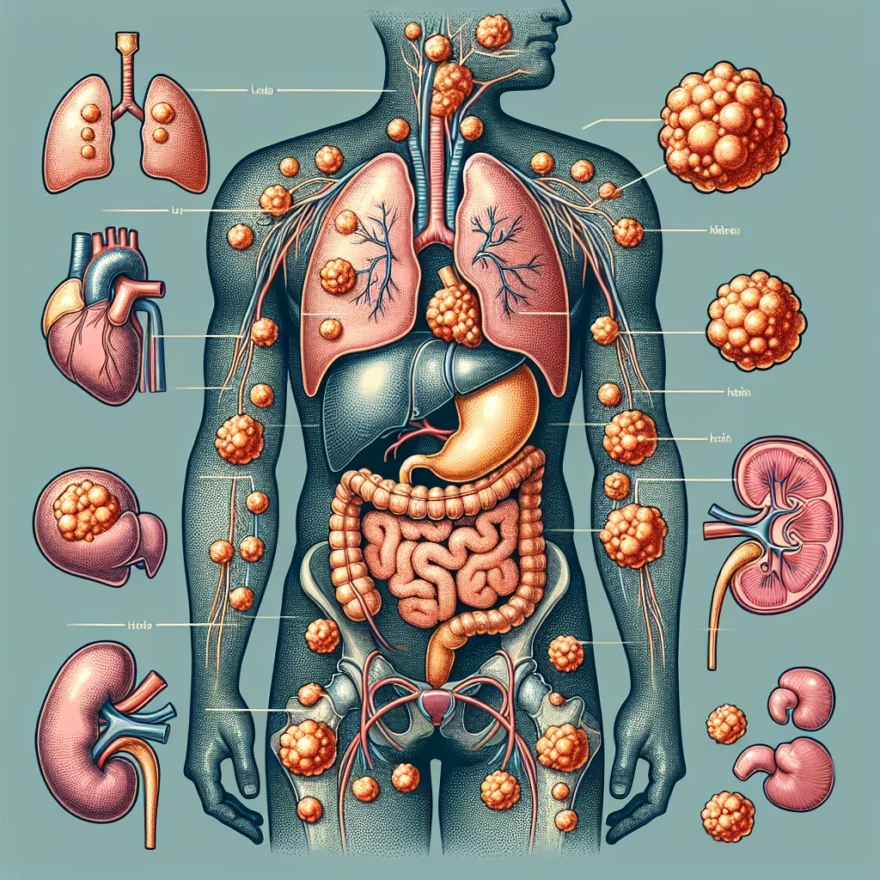
Tuberous Sclerosis Complex (TSC) is a rare genetic disorder that causes non-cancerous tumors to grow in various parts of the body. These growths can occur in the skin, brain, kidneys, eyes, heart, and lungs, where they can cause a range of health problems depending on their size and location. TSC affects approximately one in every 6,000 newborns, making it a relatively uncommon condition.
Despite the tumors being benign, they can still have significant effects on an individual’s health. For instance, brain tumors can lead to seizures, developmental delay, intellectual disability, and autism. Kidney tumors can cause hypertension and kidney failure. Lung tumors can lead to a progressive loss of lung function, whereas heart tumors, though usually benign, can cause serious problems if they obstruct blood flow.
The name “Tuberous Sclerosis” comes from the characteristic tuber or potato-like nodules that develop in the brain. These tubers can calcify with age and become hard, resembling sclerosis. It’s important to note that the course of TSC can vary widely among individuals, even within the same family. Some people may have mild symptoms or go undiagnosed, while others may experience serious complications.
Understanding the nature of TSC, its causes, symptoms, diagnosis, and treatment options can be instrumental in managing this complex disorder, improving the quality of life for those affected, and advancing research in this field.
Table of contents
Causes and Risk Factors of Tuberous Sclerosis
Tuberous Sclerosis Complex (TSC) is a genetic disorder, meaning it is caused by changes or mutations in genes. Specifically, it is linked to mutations in either the TSC1 or TSC2 gene. These genes produce proteins that act as growth suppressors, preventing cells from growing and dividing too rapidly or in an uncontrolled manner. When either of these genes is mutated, it can lead to the growth of noncancerous tumors in multiple organs of the body, a hallmark of Tuberous Sclerosis.
Most people with TSC inherit the mutated gene from a parent who has the disorder. This is known as an autosomal dominant pattern of inheritance, where only one copy of the altered gene in each cell is sufficient to cause the disorder. However, some cases result from new mutations in the gene and occur in people with no history of the disorder in their family. These are called sporadic cases.
While having a parent with Tuberous Sclerosis increases the risk of a child developing the disorder, it’s important to note that the severity of the symptoms can vary widely among family members. This is due to a phenomenon called variable expressivity, where the same genetic mutation can cause different symptoms or disease characteristics in different people.
It’s also worth noting that people with Tuberous Sclerosis are at increased risk of developing other health problems. These can include intellectual disability, developmental delay, and behavioral problems. Additionally, the presence of tumors in vital organs like the brain, heart, kidneys, eyes, lungs, and skin can lead to a range of complications, depending on their size, location, and rate of growth.
Despite the genetic nature of TSC, there are currently no known lifestyle or environmental risk factors that increase the likelihood of developing this disorder. The primary risk factor is having a family history of the disorder or being the carrier of a TSC1 or TSC2 gene mutation.
Symptoms of Tuberous Sclerosis
Tuberous Sclerosis is a complex genetic disorder that can affect multiple organs in the body. The symptoms of this condition can vary widely from person to person, depending on which organs are affected and the severity of the disease. Here are some common symptoms associated with Tuberous Sclerosis:
Skin abnormalities:
One of the most visible signs of Tuberous Sclerosis is the presence of skin abnormalities. These can include patches of thickened, rough, or discolored skin, known as facial angiofibromas or forehead plaques. Additionally, individuals with Tuberous Sclerosis may develop small, harmless growths on the skin, called fibromas or shagreen patches.
Seizures:
Seizures are a common symptom of Tuberous Sclerosis and can occur in both children and adults. These seizures can range from mild to severe and may present as staring spells, muscle jerking, or loss of consciousness. It is important for individuals with Tuberous Sclerosis to work closely with a healthcare professional to manage and control their seizures.
Developmental delays:
Tuberous Sclerosis can impact a person’s cognitive and developmental abilities. Children with the condition may experience delays in reaching developmental milestones such as sitting, crawling, or walking. They may also have learning difficulties, intellectual disabilities, or behavioral problems. Early intervention and specialized education programs can help support their development.
Cardiac complications:
In some cases, Tuberous Sclerosis can affect the heart, leading to cardiac complications. These can include arrhythmias (abnormal heart rhythms), structural abnormalities, or the formation of noncancerous tumors in the heart. Regular cardiac evaluations are essential for individuals with Tuberous Sclerosis to monitor their heart health.
Kidney problems:
Tuberous Sclerosis can also affect the kidneys, causing the growth of noncancerous tumors called renal angiomyolipomas. These tumors can lead to complications such as high blood pressure or kidney dysfunction. Regular monitoring of kidney function and imaging studies can help detect and manage these issues.
Lung complications:
In rare cases, Tuberous Sclerosis can impact the lungs, leading to the growth of cysts or noncancerous tumors. These abnormalities can cause breathing difficulties, recurrent pneumothorax (collapsed lung), or infections. Regular pulmonary evaluations are important to monitor lung health in individuals with Tuberous Sclerosis.
It is important to note that not all individuals with Tuberous Sclerosis will experience all of these symptoms. The severity and combination of symptoms can vary greatly. If you or a loved one are experiencing any of these symptoms, it is essential to consult with a healthcare professional for a proper diagnosis and appropriate management.
Diagnosing Tuberous Sclerosis
Tuberous Sclerosis, a Genetic Disorder with Tumor Growth in Multiple Organs, can be a challenging condition to diagnose due to its wide range of symptoms and the potential involvement of various organs. Diagnosing Tuberous Sclerosis typically involves a combination of medical history evaluation, physical examination, imaging tests, and genetic testing.
Medical History Evaluation:
When a patient presents with symptoms that may be indicative of Tuberous Sclerosis, the first step in the diagnostic process is a thorough medical history evaluation. The healthcare provider will inquire about any symptoms the patient is experiencing, as well as any family history of Tuberous Sclerosis or related conditions. This information helps to establish a baseline understanding of the patient’s health and aids in determining the appropriate diagnostic tests to be conducted.
Physical Examination:
Following the medical history evaluation, a physical examination is performed to assess the presence of any physical signs or symptoms associated with Tuberous Sclerosis. The healthcare provider will carefully examine the skin, looking for the characteristic facial angiofibromas (small red bumps) and hypomelanotic macules (light-colored patches). They will also evaluate the presence of any other skin abnormalities, such as shagreen patches (thickened, pebbly areas of skin) or subungual fibromas (benign tumors under the nails). In addition to the skin examination, the provider will also assess other organ systems, such as the heart, lungs, kidneys, and brain, for any potential abnormalities.
Imaging Tests:
Imaging tests are crucial in diagnosing Tuberous Sclerosis, as they help identify the presence of tumors or other abnormalities in various organs. One commonly used imaging technique is an MRI (Magnetic Resonance Imaging) scan, which provides detailed images of the brain and other organs. An MRI can help detect the presence of cortical tubers (abnormal growths in the brain), subependymal nodules (small tumors in the brain), or angiomyolipomas (benign kidney tumors). Additionally, an ultrasound may be performed to assess the kidneys for the presence of angiomyolipomas.
Genetic Testing:
Genetic testing plays a vital role in confirming a diagnosis of Tuberous Sclerosis. A blood sample is collected from the patient, and genetic testing is performed to identify mutations in the TSC1 or TSC2 genes, which are associated with Tuberous Sclerosis. Detecting these mutations helps to establish a definitive diagnosis and can also aid in determining the severity of the condition.
In some cases, a diagnosis of Tuberous Sclerosis may be made based on the presence of specific clinical criteria, even without genetic testing. These criteria, known as the “Revised Diagnostic Criteria for Tuberous Sclerosis Complex,” take into account a combination of clinical features, such as facial angiofibromas, cortical tubers, and cardiac rhabdomyomas, among others.
It is important to note that Tuberous Sclerosis is a complex disorder, and the diagnostic process may vary depending on the individual’s symptoms and medical history. Therefore, it is crucial to consult with a healthcare professional who specializes in genetic disorders and has experience in diagnosing and managing Tuberous Sclerosis.
In the next section, we will explore the various treatment options available for individuals diagnosed with Tuberous Sclerosis.
Treatment Options for Tuberous Sclerosis
Tuberous Sclerosis is a genetic disorder characterized by the growth of benign tumors in multiple organs of the body. While there is currently no cure for Tuberous Sclerosis, there are various treatment options available to manage the symptoms and improve the quality of life for individuals with this condition.
Medications
Medications are commonly used to help control the symptoms associated with Tuberous Sclerosis. Antiepileptic drugs (AEDs) are often prescribed to manage seizures, which are a common symptom of this disorder. Examples of AEDs that may be used include carbamazepine, valproic acid, and vigabatrin.
In addition to AEDs, medications such as everolimus and sirolimus have shown promising results in reducing the size of tumors associated with Tuberous Sclerosis. These medications work by inhibiting the mTOR pathway, which plays a role in the growth of these tumors.
Surgical Interventions
In some cases, surgical intervention may be necessary to manage complications of Tuberous Sclerosis. For example, if tumors in the brain are causing seizures that do not respond to medication, a surgical procedure called a resection may be performed to remove the affected tissue.
Surgery may also be considered to remove tumors in other organs such as the kidneys or lungs, especially if they are causing significant symptoms or affecting the normal functioning of the organ.
Interventional Procedures
Interventional procedures, such as embolization, may be used to treat specific symptoms associated with Tuberous Sclerosis. For instance, if an individual has a tumor that is causing excessive bleeding or affecting the blood flow in a particular organ, embolization can be performed to block the blood vessels supplying the tumor and reduce its size.
Behavioral and Educational Interventions
Individuals with Tuberous Sclerosis may benefit from behavioral and educational interventions to address developmental delays and cognitive impairments. Early intervention programs, speech therapy, occupational therapy, and special education services can all play a crucial role in supporting individuals with Tuberous Sclerosis to reach their full potential.
Supportive Therapies
Supportive therapies can help manage the symptoms and improve the overall well-being of individuals with Tuberous Sclerosis. These may include physical therapy to improve motor skills, counseling to address emotional and psychological challenges, and dietary modifications to manage specific symptoms or side effects of medications.
It is important to note that the treatment approach for Tuberous Sclerosis may vary depending on the individual and the specific symptoms they experience. A multidisciplinary team, including neurologists, geneticists, dermatologists, and other specialists, is often involved in the management and treatment of this condition.
Living with Tuberous Sclerosis
Tuberous Sclerosis is a complex genetic disorder that can have a significant impact on the lives of those affected. Living with Tuberous Sclerosis requires a multidisciplinary approach, involving various healthcare professionals and support networks. Here, we will explore some of the challenges individuals with Tuberous Sclerosis may face and discuss strategies for managing the condition.
One of the primary concerns for individuals with Tuberous Sclerosis is the development and management of tumors in multiple organs. These tumors, known as hamartomas, can affect various parts of the body, including the brain, heart, kidneys, and skin. The presence of these tumors can lead to a range of symptoms and complications. It is essential for individuals with Tuberous Sclerosis to work closely with their healthcare team to monitor and address any tumor growth.
In addition to tumor growth, Tuberous Sclerosis can also cause neurological symptoms, such as seizures, developmental delays, and intellectual disabilities. These neurological challenges can significantly impact daily life and require ongoing management. Individuals with Tuberous Sclerosis may benefit from working with specialists, such as neurologists, developmental pediatricians, and therapists, to develop personalized treatment plans.
Managing the physical and cognitive symptoms of Tuberous Sclerosis often involves a combination of medication, therapies, and lifestyle modifications. Medications can help control seizures and manage other symptoms, while therapies such as occupational therapy, speech therapy, and physical therapy can support individuals in improving their daily functioning and overall quality of life.
It is crucial for individuals with Tuberous Sclerosis to have a strong support network in place. This may include family, friends, and support groups who can provide emotional support, share experiences, and offer practical assistance. Connecting with others who are going through similar experiences can be incredibly valuable in navigating the challenges of living with Tuberous Sclerosis.
Education and advocacy are also essential components of living with Tuberous Sclerosis. Individuals with the condition and their families should seek out reliable sources of information to better understand the disorder and its management. By staying informed, individuals can actively participate in their own care and make informed decisions about treatment options.
While living with Tuberous Sclerosis can present unique challenges, it is important to remember that individuals with the condition can lead fulfilling lives. With appropriate medical care, support, and self-care strategies, many individuals with Tuberous Sclerosis are able to manage their symptoms and pursue their goals and aspirations.
Ultimately, the journey of living with Tuberous Sclerosis is unique to each individual. It is crucial to work closely with healthcare professionals, seek support from loved ones, and stay informed about the latest research and treatment options. By doing so, individuals with Tuberous Sclerosis can optimize their quality of life and thrive despite the challenges they may face.
Research and Advances in Tuberous Sclerosis
Tuberous Sclerosis (TS) is a complex genetic disorder that affects multiple organs in the body, leading to the formation of noncancerous tumors. Over the years, extensive research has been conducted to better understand this condition and develop effective treatment strategies. Let’s explore some of the recent advances in the field of Tuberous Sclerosis research:
1. Genetic Studies:
Researchers have made significant progress in identifying the specific genes responsible for Tuberous Sclerosis. The discovery of TSC1 and TSC2 genes, which encode for proteins that regulate cell growth and division, has provided valuable insights into the molecular mechanisms underlying this disorder. Further genetic studies are being conducted to explore other potential genes involved in the development of Tuberous Sclerosis.
2. Animal Models:
Animal models, particularly mice and zebrafish, have played a crucial role in advancing our understanding of Tuberous Sclerosis. By manipulating the TSC1 and TSC2 genes in these models, researchers have been able to study the effects of gene mutations and develop a better understanding of the disease progression. These models have also been instrumental in testing potential therapeutic interventions.
3. Targeted Therapies:
Recent research has focused on developing targeted therapies that specifically address the underlying molecular abnormalities in Tuberous Sclerosis. One such example is the use of mTOR inhibitors, such as everolimus and sirolimus, which have shown promising results in shrinking tumors and reducing seizure frequency in individuals with Tuberous Sclerosis. Ongoing clinical trials are investigating the efficacy of these drugs and exploring other potential targeted therapies.
4. Biomarkers:
Efforts are underway to identify biomarkers that can aid in the early diagnosis and monitoring of Tuberous Sclerosis. Biomarkers are measurable indicators, such as proteins or genetic markers, that can help predict disease progression and treatment response. The discovery of reliable biomarkers would not only facilitate early intervention but also enable personalized treatment approaches for individuals with Tuberous Sclerosis.
5. Gene Therapy:
Gene therapy, a rapidly evolving field, holds great promise for the treatment of genetic disorders like Tuberous Sclerosis. Scientists are exploring innovative gene-editing techniques, such as CRISPR-Cas9, to correct the genetic mutations responsible for Tuberous Sclerosis. Although still in the experimental stages, gene therapy has the potential to revolutionize the treatment of this condition in the future.
6. Supportive Care:
While research continues to focus on finding a cure for Tuberous Sclerosis, significant efforts are also being made to improve supportive care for individuals living with this condition. This includes the development of multidisciplinary clinics that provide comprehensive medical and psychosocial support, as well as educational resources for patients, families, and healthcare professionals.
Overall, the research and advances in Tuberous Sclerosis are paving the way for a better understanding of the condition and improved treatment options. Through ongoing studies and collaborative efforts, researchers and healthcare professionals are working towards enhancing the quality of life for individuals affected by Tuberous Sclerosis.
Common Questions about Tuberous Sclerosis
Common Questions about Tuberous Sclerosis
As a genetic disorder with tumor growth in multiple organs, tuberous sclerosis can raise many questions and concerns. Here are some common questions that people often have:
1. Is tuberous sclerosis a rare condition?
Yes, tuberous sclerosis is considered a rare condition, affecting approximately 1 in 6,000 to 10,000 individuals worldwide. However, it is important to note that the severity and symptoms can vary widely among those affected.
2. Can tuberous sclerosis be inherited?
Yes, tuberous sclerosis is caused by mutations in either the TSC1 or TSC2 gene, which are inherited in an autosomal dominant pattern. This means that if one parent has the condition, there is a 50% chance of passing it on to their child.
3. What are the most common symptoms of tuberous sclerosis?
Tuberous sclerosis can affect various organs in the body, leading to a wide range of symptoms. Some of the most common symptoms include seizures, developmental delays, intellectual disabilities, skin abnormalities (such as facial angiofibromas or white patches), kidney problems, and lung complications.
4. How is tuberous sclerosis diagnosed?
Diagnosing tuberous sclerosis typically involves a combination of clinical evaluation, imaging tests (such as MRI or CT scans), genetic testing, and analysis of skin lesions or tumors. A healthcare professional with expertise in the condition can help guide the diagnostic process.
5. Are there any treatments available for tuberous sclerosis?
While there is currently no cure for tuberous sclerosis, there are various treatment options available to manage the symptoms and complications associated with the condition. Treatment may include medications to control seizures, therapies to support developmental delays, surgical interventions for specific tumors or organ involvement, and ongoing monitoring and support from a healthcare team.
6. Can individuals with tuberous sclerosis lead normal lives?
With appropriate medical care and support, many individuals with tuberous sclerosis can lead fulfilling lives. Early intervention, including therapies and educational support, can help individuals reach their full potential. However, the impact of the condition can vary, and ongoing medical management is typically required to address any complications that may arise.
7. Is there ongoing research for tuberous sclerosis?
Yes, research into tuberous sclerosis is ongoing. Scientists are continuously working to better understand the condition, identify new treatment options, and improve the quality of life for individuals affected by tuberous sclerosis. Advances in genetics, imaging technology, and targeted therapies offer hope for future advancements in the field.
It is important to consult with healthcare professionals and specialists to receive accurate and personalized information about tuberous sclerosis. Each individual’s experience with the condition may vary, and a comprehensive approach to care is crucial.