Introduction to Urticarial Vasculitis
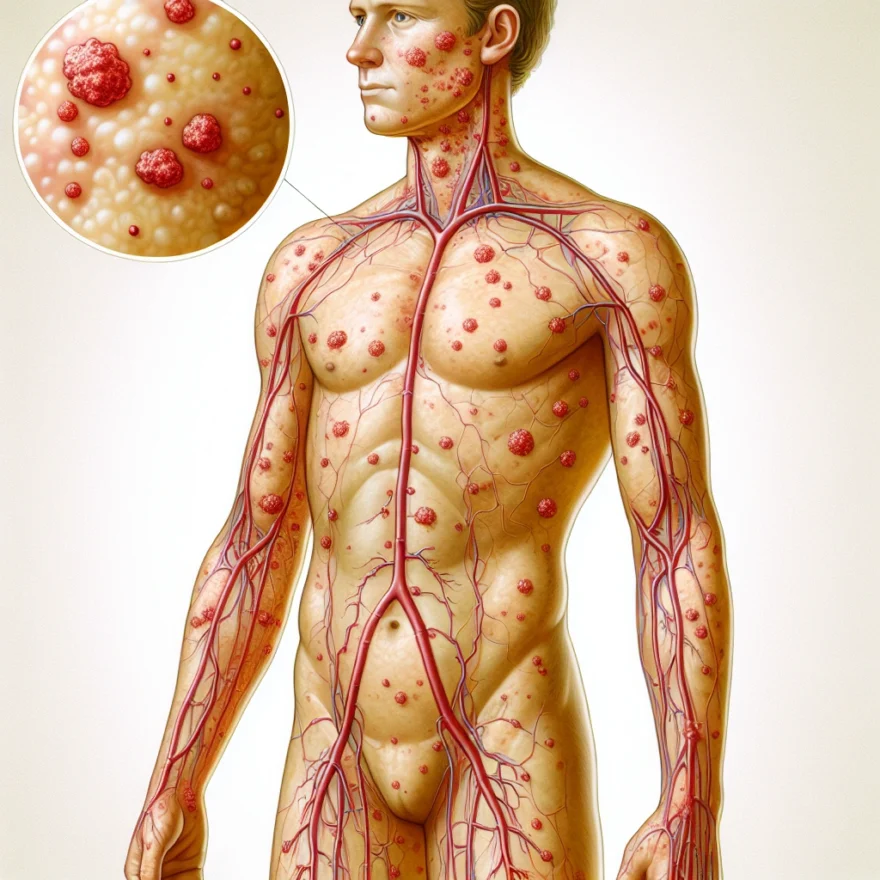
Urticarial Vasculitis is a unique and rare form of vasculitis that primarily affects the skin. Vasculitis refers to a group of disorders characterized by the inflammation of blood vessels, including veins, arteries, and capillaries. When this inflammation occurs in the small blood vessels of the skin, causing hive-like lesions, it is known as Urticarial Vasculitis.
This condition can occur at any age but is most commonly observed in adults in their middle ages. It is also seen more frequently in women than in men. The exact incidence of Urticarial Vasculitis is unknown due to its rarity, but it is estimated to affect approximately 1 in 100,000 people worldwide.
Urticarial Vasculitis can be categorized into two types: normocomplementemic and hypocomplementemic. The normocomplementemic type is more common and less severe, with symptoms limited to the skin. The hypocomplementemic type, on the other hand, is less common but more severe, often involving other organs and systems in the body.
It is important to note that Urticarial Vasculitis is not just a prolonged case of hives. While the lesions may resemble hives, they typically last longer (more than 24 hours) and often leave behind a bruise or a pigmented area. The inflammation in the blood vessels can cause pain and burning sensation, distinguishing it from ordinary hives.
Understanding Urticarial Vasculitis is crucial, not just for those who have been diagnosed with it, but also for those who may be experiencing unexplained and persistent skin lesions. Increased awareness about this condition can lead to timely diagnosis and appropriate treatment, improving the quality of life for those affected by it.
Table of contents
Causes and Risk Factors
Understanding the causes and risk factors of Urticarial Vasculitis can be complex, as this rare skin condition is still being studied by medical experts. However, some insights have been gathered that can help shed light on what may contribute to its onset.
Urticarial Vasculitis is an autoimmune disease, which means that it occurs when the body’s immune system mistakenly attacks its own cells. In the case of Urticarial Vasculitis, the immune system attacks the small blood vessels in the skin, causing inflammation and damage. This inflammation leads to the characteristic hives or ‘urticaria’ that mark the condition.
While the exact cause of Urticarial Vasculitis is unknown, it is believed that certain factors may increase a person’s risk. For instance, it has been observed that individuals with a family history of autoimmune diseases are more likely to develop the condition. This suggests a genetic component to the disease, though more research is needed to confirm this.
Other potential risk factors include existing autoimmune conditions, such as lupus or Sjögren’s syndrome. These conditions can trigger an inflammatory response in the body, which may in turn lead to Urticarial Vasculitis. Certain infections, medications, and even environmental factors such as exposure to extreme cold or heat may also trigger the condition.
It’s important to note that having one or more of these risk factors does not guarantee that a person will develop Urticarial Vasculitis. Many people with these risk factors never develop the condition, and conversely, some people with no known risk factors do. This further underscores the complexity of the disease and the need for ongoing research.
Symptoms of Urticarial Vasculitis
Urticarial vasculitis is a rare form of vasculitis that primarily affects the skin. This condition is characterized by the development of hives (urticaria) and inflammation of the blood vessels (vasculitis). The symptoms of urticarial vasculitis can vary in severity and duration, and they may come and go over time.
One of the main symptoms of urticarial vasculitis is the presence of persistent hives that last for more than 24 hours. These hives are usually red or pink in color and can be itchy or painful. Unlike ordinary hives, which typically resolve within a few hours, the hives associated with urticarial vasculitis tend to persist for longer periods of time and may leave behind a bruise-like discoloration.
In addition to hives, individuals with urticarial vasculitis may also experience other skin manifestations. These can include raised patches of skin (plaques), small red or purple spots (petechiae), and blister-like lesions (bullae). These skin lesions can be localized to certain areas of the body or may be more widespread.
Another common symptom of urticarial vasculitis is joint pain (arthralgia). This can affect multiple joints in the body and may be associated with swelling and stiffness. The joint pain can range from mild to severe and can significantly impact an individual’s mobility and quality of life.
Some individuals with urticarial vasculitis may also experience systemic symptoms, which can affect various organs in the body. These can include fever, fatigue, weight loss, and muscle aches. Systemic symptoms are more commonly seen in individuals with a more severe form of the condition.
It’s important to note that the symptoms of urticarial vasculitis can vary from person to person, and not all individuals will experience the same set of symptoms. Additionally, the severity and duration of symptoms can also fluctuate over time, with periods of remission and flare-ups.
If you suspect that you may have urticarial vasculitis, it is important to consult with a healthcare professional for proper diagnosis and management of your symptoms. A thorough evaluation, including a physical examination, medical history review, and possibly skin or tissue biopsy, may be necessary to confirm the diagnosis.
Once diagnosed, treatment options for urticarial vasculitis can include medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), antihistamines, corticosteroids, and immunosuppressive agents. The specific treatment plan will depend on the severity of symptoms and the individual’s overall health.
Overall, understanding the symptoms of urticarial vasculitis is crucial for early detection and appropriate management of this rare condition. By recognizing the signs and seeking medical attention, individuals with urticarial vasculitis can work with healthcare professionals to develop a personalized treatment plan and improve their quality of life.
Diagnosis of Urticarial Vasculitis
Diagnosing urticarial vasculitis can be a complex process, as it shares symptoms with other skin conditions. However, there are specific criteria that doctors use to determine whether a patient has urticarial vasculitis.
When a patient presents with symptoms suggestive of urticarial vasculitis, the first step in the diagnostic process is a thorough physical examination. The doctor will carefully examine the skin for characteristic signs, such as raised red or purple lesions that resemble hives. They will also look for any signs of inflammation or discoloration.
In addition to the physical examination, the doctor will also take a detailed medical history. They will ask about the duration and frequency of the symptoms, any triggers that may be associated with the flare-ups, and any previous medical conditions or medications that the patient has taken.
After the initial assessment, the doctor may order several diagnostic tests to confirm the diagnosis of urticarial vasculitis. These tests may include:
- Skin biopsy: A small sample of the affected skin is taken and examined under a microscope. This can help determine if there is inflammation in the blood vessels.
- Blood tests: Blood tests can help identify any underlying autoimmune or systemic diseases that may be contributing to the urticarial vasculitis. These tests may include complete blood count (CBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and complement levels.
- Immunological tests: These tests can detect the presence of specific antibodies, such as antinuclear antibodies (ANA) or anti-neutrophil cytoplasmic antibodies (ANCA), which are associated with autoimmune conditions.
- Other imaging tests: In some cases, imaging tests such as ultrasound or angiography may be performed to evaluate the blood vessels and rule out other vascular disorders.
It is important to note that the diagnosis of urticarial vasculitis can be challenging, and it may require consultation with a dermatologist or a rheumatologist who specializes in vasculitis. These specialists have the expertise to interpret the results of the diagnostic tests and differentiate urticarial vasculitis from other similar conditions.
Once a diagnosis of urticarial vasculitis is confirmed, the doctor will work closely with the patient to develop an appropriate treatment plan.
Treatment Options for Urticarial Vasculitis
Urticarial Vasculitis, being a rare form of vasculitis that affects the skin, requires appropriate treatment to manage its symptoms and prevent complications. The treatment options for Urticarial Vasculitis may vary depending on the severity of the condition and individual patient factors. Here are some common treatment approaches that healthcare professionals may consider:
1. Medications:
– Nonsteroidal anti-inflammatory drugs (NSAIDs): Mild cases of Urticarial Vasculitis can often be managed with over-the-counter NSAIDs like ibuprofen or naproxen to reduce inflammation and relieve pain.
– Antihistamines: These medications can help alleviate itching and reduce the frequency and severity of hives associated with Urticarial Vasculitis. Non-drowsy antihistamines like cetirizine or loratadine are commonly prescribed.
– Corticosteroids: In more severe cases, corticosteroids may be prescribed to suppress the immune system and reduce inflammation. Oral corticosteroids like prednisone or intravenous corticosteroids may be used depending on the severity of the symptoms.
– Immunosuppressants: If corticosteroids alone are not sufficient, immunosuppressant drugs like azathioprine or methotrexate may be prescribed to further suppress the immune response.
2. Topical Treatments:
– Topical corticosteroids: For localized symptoms, such as skin rashes or hives, topical corticosteroids in the form of creams or ointments may be prescribed to reduce inflammation and itching.
– Calamine lotion: This soothing lotion can provide relief from itching and help soothe the skin affected by Urticarial Vasculitis.
3. Avoidance of Triggers:
– Identifying and avoiding triggers that worsen the symptoms of Urticarial Vasculitis is an important part of managing the condition. Common triggers may include certain medications, exposure to extreme temperatures, stress, or certain foods. Keeping a diary to track potential triggers can be helpful in managing the condition.
4. Cold Compresses:
– Applying cold compresses or ice packs to affected areas can help reduce inflammation, relieve itching, and provide temporary relief from discomfort.
5. Phototherapy:
– In some cases, phototherapy may be recommended as a treatment option. This involves exposing the skin to specific wavelengths of light to reduce inflammation and improve symptoms.
It is important to note that the treatment plan for Urticarial Vasculitis should be individualized based on the patient’s specific needs and the severity of their symptoms. Regular follow-up appointments with a healthcare professional are crucial to monitor the effectiveness of the treatment and make any necessary adjustments.
Always consult with a qualified healthcare professional before starting any new treatment or making changes to an existing treatment plan. They will be able to provide personalized advice and guidance based on your unique medical history and condition.
Living with Urticarial Vasculitis
Living with Urticarial Vasculitis
Living with urticarial vasculitis can be challenging, as it is a chronic condition that affects the skin and can cause discomfort and pain. However, with proper management and lifestyle adjustments, individuals with urticarial vasculitis can lead fulfilling lives. Here are some important aspects to consider when living with this condition:
1. Self-Care and Skin Protection:
– It is crucial to take good care of your skin to minimize flare-ups and prevent further damage. This includes keeping the skin clean and moisturized.
– Use gentle skincare products that are free from harsh chemicals, fragrances, and irritants.
– Protect your skin from excessive sun exposure by wearing sunscreen with a high SPF and protective clothing.
– Avoid extreme temperatures, as both extreme heat and cold can trigger symptoms.
2. Managing Triggers:
– Identifying and avoiding triggers can help in preventing or reducing the frequency and severity of urticarial vasculitis flare-ups.
– Common triggers include certain medications, infections, exposure to cold temperatures, stress, and pressure on the skin.
– Keeping a diary to track your symptoms and potential triggers can be helpful in identifying patterns and making necessary lifestyle adjustments.
3. Medication and Treatment:
– Work closely with your healthcare team to develop an individualized treatment plan.
– Medications such as antihistamines, nonsteroidal anti-inflammatory drugs (NSAIDs), and corticosteroids may be prescribed to manage symptoms and reduce inflammation.
– In some cases, immunosuppressive medications may be necessary to control the immune system’s response.
– Follow your prescribed medication regimen and communicate any concerns or side effects to your healthcare provider.
4. Emotional Support:
– Living with a chronic condition like urticarial vasculitis can take a toll on your emotional well-being.
– Seek support from friends, family, or support groups who can provide understanding and empathy.
– Consider speaking with a mental health professional who can help you cope with the emotional challenges associated with the condition.
5. Regular Follow-ups:
– It is important to have regular follow-up appointments with your healthcare provider to monitor your condition and adjust your treatment plan if needed.
– Keep track of your symptoms and any changes in your condition to discuss with your healthcare team during these appointments.
6. Healthy Lifestyle:
– Maintaining a healthy lifestyle can help support your overall well-being and manage the symptoms of urticarial vasculitis.
– Eat a balanced diet rich in fruits, vegetables, whole grains, and lean proteins.
– Engage in regular exercise, as it can help improve circulation and reduce inflammation.
– Get adequate rest and practice stress-management techniques such as meditation or yoga.
Remember, every individual’s experience with urticarial vasculitis can vary, and it is important to work closely with your healthcare team to develop a personalized management plan. With proper care and support, it is possible to lead a fulfilling life despite the challenges posed by this rare form of vasculitis affecting the skin.
Common Questions about Urticarial Vasculitis
Common Questions about Urticarial Vasculitis
Urticarial vasculitis is a rare form of vasculitis that affects the skin, causing itchy hives and inflammation. As with any medical condition, there are often questions that arise. Here are some common questions about urticarial vasculitis:
1. What causes urticarial vasculitis?
The exact cause of urticarial vasculitis is unknown in many cases. However, it can be associated with autoimmune disorders such as lupus or rheumatoid arthritis. It can also be triggered by certain medications, infections, or environmental factors.
2. What are the symptoms of urticarial vasculitis?
The main symptom of urticarial vasculitis is the development of hives that last longer than 24 hours and leave behind a bruise-like appearance. Other symptoms may include joint pain, fever, fatigue, and abdominal pain. It is important to note that symptoms can vary from person to person.
3. How is urticarial vasculitis diagnosed?
Diagnosing urticarial vasculitis can be challenging as it shares similarities with other skin conditions. A thorough physical examination, medical history review, and blood tests may be conducted to rule out other causes and confirm the diagnosis. In some cases, a skin biopsy may be necessary.
4. What are the treatment options for urticarial vasculitis?
Treatment for urticarial vasculitis aims to relieve symptoms and manage the underlying cause, if identified. This may involve the use of antihistamines, nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, or immunosuppressant medications. Avoiding triggers, such as certain medications or environmental factors, may also be recommended.
5. Can urticarial vasculitis be cured?
Urticarial vasculitis is a chronic condition, and while there is no known cure, it can be managed effectively with proper medical care. With appropriate treatment and lifestyle modifications, many individuals with urticarial vasculitis are able to lead normal lives and keep their symptoms under control.
6. How can I live with urticarial vasculitis?
Living with urticarial vasculitis may require making certain adjustments to your lifestyle. It is important to work closely with your healthcare provider to develop an individualized treatment plan. Taking steps to reduce stress, avoiding triggers, protecting your skin from extreme temperatures, and maintaining a healthy lifestyle can also help manage the condition.
7. Are there any complications associated with urticarial vasculitis?
In some cases, urticarial vasculitis can lead to complications such as skin ulcers, joint damage, or kidney involvement. Regular follow-up appointments with your healthcare provider are essential to monitor your condition and detect any potential complications early on.
8. Can urticarial vasculitis be prevented?
Since the exact cause of urticarial vasculitis is often unknown, it is difficult to prevent the condition entirely. However, avoiding known triggers, managing underlying autoimmune conditions, and maintaining a healthy lifestyle can help reduce the frequency and severity of flare-ups.
It is important to consult with a healthcare professional for personalized advice and guidance regarding urticarial vasculitis.
Conclusion
In conclusion, Urticarial Vasculitis is a rare form of vasculitis that primarily affects the skin. It is characterized by the presence of hives or urticaria-like lesions, which can be accompanied by other systemic symptoms.
The causes of Urticarial Vasculitis are not fully understood, but it is believed to be an autoimmune condition. It can occur in isolation or as a result of an underlying systemic disease. Certain risk factors, such as female gender and middle age, have also been associated with the development of Urticarial Vasculitis.
The symptoms of Urticarial Vasculitis can vary from person to person, but commonly include persistent hives, joint pain, and swelling. In severe cases, it can lead to organ involvement and systemic complications.
Diagnosing Urticarial Vasculitis can be challenging, as it requires a thorough evaluation of the patient’s medical history, physical examination, and laboratory tests. Skin biopsies are often necessary to confirm the diagnosis.
Treatment options for Urticarial Vasculitis aim to control the symptoms and prevent complications. This may involve the use of antihistamines, nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and other immunosuppressive medications.
Living with Urticarial Vasculitis can be challenging, as the condition can be chronic and unpredictable. It is important for patients to work closely with their healthcare providers to manage symptoms, avoid triggers, and monitor for any signs of disease progression.
Common questions about Urticarial Vasculitis include inquiries about the long-term prognosis, the potential for disease remission, and the impact on daily life. It is important for individuals with Urticarial Vasculitis to seek support from healthcare professionals, patient support groups, and loved ones.
In summary, Urticarial Vasculitis is a rare form of vasculitis that affects the skin. While it can be challenging to diagnose and manage, with proper medical care and support, individuals with Urticarial Vasculitis can lead fulfilling lives and effectively manage their symptoms.