Introduction to Vogt-Koyanagi-Harada Syndrome
Imagine your body’s immune system, that loyal guardian designed to protect you from harmful foreign invaders, suddenly turns against you. That’s what happens in an autoimmune disorder, and Vogt-Koyanagi-Harada (VKH) Syndrome is one such condition. A rare, multisystem autoimmune disorder, VKH Syndrome primarily affects the eyes, but can also involve the ears, skin, and the meninges – the protective layers covering the brain and spinal cord.
Named after three physicians who described the condition in the early 20th century, Vogt-Koyanagi-Harada Syndrome is characterized by chronic, bilateral, diffuse uveitis. Uveitis refers to inflammation of the uvea, the middle layer of the eye, which includes the iris, ciliary body, and choroid. This inflammation can cause a variety of vision-threatening complications, including cataracts, glaucoma, and retinal detachment.
While VKH Syndrome is considered rare, it is one of the leading causes of non-infectious uveitis worldwide. It is more common in certain populations, such as people of Asian, Hispanic, and Native American descent. The disease typically manifests in young adulthood, with a slight female predominance.
Despite being identified over a century ago, VKH Syndrome remains a complex and poorly understood condition. Its rarity and the lack of a definitive diagnostic test often lead to delays in diagnosis and treatment, which can result in significant vision loss. However, with early recognition and appropriate treatment, the prognosis for VKH Syndrome can be quite favorable.
Table of contents
- Introduction to Vogt-Koyanagi-Harada Syndrome
- Understanding Autoimmune Disorders
- How Vogt-Koyanagi-Harada Syndrome Affects the Eyes
- Symptoms of Vogt-Koyanagi-Harada Syndrome
- Causes and Risk Factors of Vogt-Koyanagi-Harada Syndrome
- Diagnosis of Vogt-Koyanagi-Harada Syndrome
- Treatment and Management of Vogt-Koyanagi-Harada Syndrome
- Living with Vogt-Koyanagi-Harada Syndrome
- Latest Research on Vogt-Koyanagi-Harada Syndrome
- Frequently Asked Questions about Vogt-Koyanagi-Harada Syndrome
Understanding Autoimmune Disorders
Before delving into the specifics of Vogt-Koyanagi-Harada Syndrome, it’s critical to have a clear understanding of autoimmune disorders, the umbrella under which this condition falls. The human immune system is a complex network of cells and proteins designed to defend the body against harmful invaders such as bacteria, viruses, and foreign substances. In a healthy immune system, a delicate balance is maintained to ensure that these invaders are effectively combated without causing harm to the body’s own cells.
However, in an autoimmune disorder, this balance is disrupted. The immune system mistakenly identifies the body’s own cells as foreign invaders and mounts an attack against them. This results in inflammation and damage to the affected tissues and organs. The exact cause of this misidentification is not completely understood, but it is believed to involve a combination of genetic and environmental factors.
Autoimmune disorders can affect any part of the body, and the symptoms and severity can vary greatly depending on the specific disorder and the individual. Some autoimmune disorders target one specific organ, such as Type 1 diabetes, which affects the pancreas. Others, like lupus, can affect multiple organs and systems in the body.
Vogt-Koyanagi-Harada Syndrome is one such autoimmune disorder that primarily affects the eyes, but can also involve other parts of the body such as the skin, the inner ear, and the meninges – the protective membranes covering the brain and spinal cord. Like other autoimmune disorders, it is characterized by periods of active disease followed by periods of remission. Understanding this context of autoimmune disorders is essential to comprehending the complexities of Vogt-Koyanagi-Harada Syndrome.
How Vogt-Koyanagi-Harada Syndrome Affects the Eyes
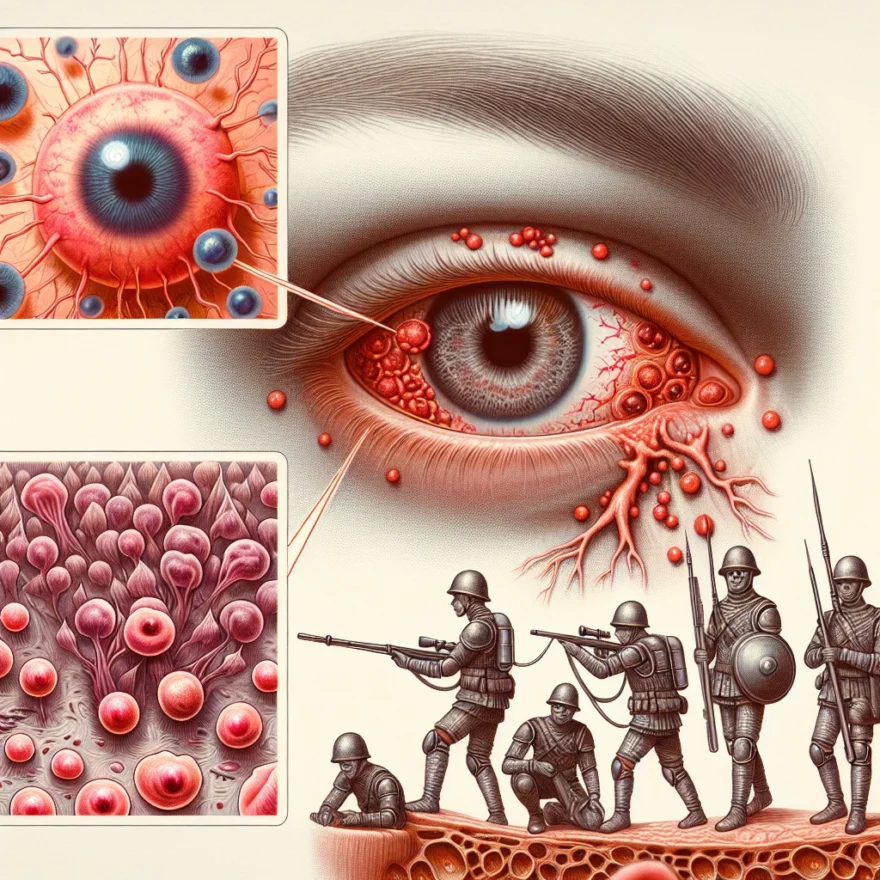
Vogt-Koyanagi-Harada Syndrome (VKH) is an autoimmune disorder that primarily affects the eyes, among other parts of the body. This syndrome is characterized by inflammation in various structures of the eye, leading to vision problems and potential long-term complications if left untreated.
The inflammation associated with VKH primarily affects the uvea, which is the middle layer of the eye that includes the iris, choroid, and ciliary body. The uvea plays a crucial role in providing nourishment to the retina and maintaining the overall health of the eye.
In VKH, the inflammation in the uvea can lead to several ocular manifestations. One of the most common symptoms is uveitis, which refers to the inflammation of the uvea. Uveitis can cause redness, pain, and sensitivity to light. It may also result in blurred vision and the perception of floaters or small specks in the visual field.
Another way VKH affects the eyes is through the development of choroidal effusions. Choroidal effusions occur when fluid accumulates in the choroid, leading to a separation between the choroid and the overlying retina. This can result in a condition called serous retinal detachment, which causes vision loss and distortion.
In some cases, VKH may also cause inflammation in the optic nerve, leading to optic disc swelling. This can further impair vision and may result in a condition known as papillitis.
Additionally, VKH can affect the pigmentation of the eyes. People with VKH may experience changes in the color of their irises, such as heterochromia, where the irises of both eyes have different colors. This occurs due to the destruction of melanocytes, which are responsible for producing pigment in the iris.
It is important to note that VKH can affect both eyes simultaneously, although the severity of symptoms may vary between the two eyes. Prompt diagnosis and treatment are crucial to minimize the potential damage to the eyes and preserve visual function.
In the next section, we will explore the specific symptoms associated with Vogt-Koyanagi-Harada Syndrome and how they can be recognized.
Symptoms of Vogt-Koyanagi-Harada Syndrome
Vogt-Koyanagi-Harada Syndrome (VKH) is an autoimmune disorder that primarily affects the eyes but can also involve other organs such as the skin, hair, and nervous system. The syndrome is characterized by a chronic inflammation of the uveal tract, which includes the iris, ciliary body, and choroid. This inflammation can lead to a variety of symptoms that can significantly impact a person’s vision and overall quality of life.
One of the key symptoms of Vogt-Koyanagi-Harada Syndrome is a sudden or gradual loss of vision. This can occur in one or both eyes and may be accompanied by blurred or decreased vision. Patients may also experience sensitivity to light (photophobia) and have difficulty adjusting to changes in lighting conditions.
In addition to vision problems, VKH can cause inflammation of the eye tissues, leading to redness, pain, and discomfort. Patients may also develop floaters, which are small specks or spots that appear to float in the field of vision. These floaters are caused by the presence of inflammatory cells in the vitreous, the gel-like substance that fills the center of the eye.
Another common symptom of VKH is the presence of skin and hair abnormalities. Patients may notice changes in their skin pigmentation, such as patches of hyperpigmentation or depigmentation. The hair may also become prematurely gray or even fall out in some cases.
Neurological symptoms can also occur in some individuals with VKH. These may include headaches, dizziness, and meningitis-like symptoms such as fever, stiff neck, and nausea. In rare cases, more severe neurological complications can arise, such as seizures or paralysis.
It is important to note that the symptoms of VKH can vary from person to person and may change over time. Some individuals may only experience mild symptoms, while others may have more severe and persistent manifestations of the syndrome.
If you are experiencing any of these symptoms or suspect you may have Vogt-Koyanagi-Harada Syndrome, it is crucial to seek medical attention promptly. Early diagnosis and treatment can help manage the symptoms and prevent potential complications.
Causes and Risk Factors of Vogt-Koyanagi-Harada Syndrome
Vogt-Koyanagi-Harada Syndrome (VKH) is an autoimmune disorder that primarily affects the eyes. While the exact cause of VKH is still unknown, researchers believe that a combination of genetic and environmental factors play a role in its development. Understanding the potential causes and risk factors associated with VKH can help shed light on this complex condition.
Genetic Factors
Studies have suggested a genetic predisposition to VKH, as the syndrome tends to occur more frequently in certain ethnic groups, such as Asian, Native American, and Hispanic populations. Specific genes associated with immune system regulation and melanocyte function have been identified as potential contributors to VKH development. However, further research is needed to fully understand the genetic mechanisms involved.
Environmental Triggers
Environmental factors may also play a role in triggering VKH in individuals with a genetic susceptibility. Infections, particularly viral and bacterial infections, have been linked to the onset of VKH. In some cases, the body’s immune response to these infections may mistakenly attack the melanocytes in the eyes, leading to the development of VKH symptoms. Other potential triggers include exposure to certain chemicals or toxins, although more research is needed to establish a definitive link.
Immune System Dysfunction
VKH is classified as an autoimmune disorder, which means that the body’s immune system mistakenly attacks healthy tissues. In the case of VKH, the immune system targets melanocytes, which are cells responsible for producing pigment in the eyes, skin, and hair. The exact reasons behind this immune system dysfunction are not fully understood, but it is believed to involve a combination of genetic and environmental factors.
Heredity
While the exact mode of inheritance for VKH is not clear, there is evidence to suggest that there may be a hereditary component to the syndrome. Family history of VKH or other autoimmune disorders may increase the risk of developing the condition. However, it is important to note that having a family history does not guarantee the development of VKH, as other factors are likely involved.
Gender and Age
VKH has been found to occur more frequently in females than males, although the reason for this gender disparity is still unclear. Additionally, VKH tends to affect individuals between the ages of 20 and 50, with the average age of onset being in the late 30s. However, VKH can occur at any age, including in children and older adults.
Diagnosis of Vogt-Koyanagi-Harada Syndrome
Vogt-Koyanagi-Harada Syndrome (VKH) is a rare autoimmune disorder that primarily affects the eyes but can also involve other organs such as the skin, hair, and nervous system. Diagnosing VKH can be challenging as its symptoms can mimic other eye conditions. A thorough evaluation by a healthcare professional is necessary to make an accurate diagnosis.
The diagnostic process for VKH involves a combination of medical history, physical examination, and specialized tests. The healthcare provider will typically begin by asking the patient about their symptoms, including any visual changes, eye pain, or sensitivity to light. They will also inquire about any other symptoms that may suggest involvement of other organs.
During the physical examination, the healthcare provider will carefully examine the eyes, looking for signs such as redness, swelling, or inflammation. They may also perform a visual acuity test to assess the patient’s vision. In some cases, the provider may use a slit lamp microscope to examine the structures at the front of the eye in more detail.
To confirm the diagnosis of VKH, the healthcare provider may order additional tests. One common test is called an ophthalmoscopy, which allows the provider to visualize the back of the eye, including the retina and optic nerve. This can help identify any characteristic changes associated with VKH, such as swelling or fluid accumulation.
Another important test is called a fluorescein angiography. During this test, a special dye is injected into the patient’s arm, and a series of photographs are taken as the dye circulates through the blood vessels in the eyes. This test helps to evaluate the blood flow in the retina and can reveal any abnormalities or leakage that may be indicative of VKH.
In some cases, the healthcare provider may also order laboratory tests to support the diagnosis of VKH. These tests may include blood tests to check for specific antibodies or markers of inflammation, as well as a lumbar puncture (spinal tap) to analyze the cerebrospinal fluid for signs of inflammation.
It is important to note that the diagnosis of VKH is based on a combination of clinical findings and test results. The healthcare provider will consider the patient’s symptoms, physical examination findings, and test results to make an accurate diagnosis.
If VKH is suspected, it is crucial to consult with an ophthalmologist or a specialist in uveitis, as they have expertise in diagnosing and managing this condition. Early diagnosis and treatment are essential to prevent complications and preserve vision.
Treatment and Management of Vogt-Koyanagi-Harada Syndrome
Once a diagnosis of Vogt-Koyanagi-Harada Syndrome (VKH) is confirmed, treatment and management strategies can be implemented to help control the symptoms and prevent further complications. The main goals of treatment are to reduce inflammation, preserve vision, and manage associated symptoms.
1. Medications:
One of the primary approaches in managing VKH is the use of medications. Corticosteroids, such as prednisone, are commonly prescribed to reduce inflammation and suppress the immune response. These medications are usually administered orally or through intravenous injections in severe cases. Over time, the dosage is gradually tapered down to the lowest effective level to minimize side effects.
In some cases, immunomodulatory drugs may be prescribed in combination with corticosteroids to help maintain long-term remission and reduce the need for high doses of steroids. These drugs, including methotrexate, azathioprine, and cyclosporine, work by suppressing the immune system and preventing further attacks on the eyes.
2. Ophthalmic Treatment:
As VKH primarily affects the eyes, ophthalmic treatment plays a crucial role in managing the condition. Eye drops containing corticosteroids or nonsteroidal anti-inflammatory drugs (NSAIDs) may be prescribed to reduce inflammation and alleviate symptoms such as redness, pain, and light sensitivity. These eye drops are typically used multiple times a day and should be administered as directed by the ophthalmologist.
In some cases, the ophthalmologist may recommend the use of cycloplegic agents, which help relax the muscles of the eye and reduce pain and discomfort. These agents also prevent the formation of adhesions between the iris and lens, which can lead to complications like cataracts and glaucoma.
3. Follow-up Care:
Regular follow-up appointments with an ophthalmologist are essential for monitoring the progression of VKH and adjusting the treatment plan accordingly. During these visits, the ophthalmologist will assess visual acuity, examine the eyes for any signs of inflammation or complications, and make any necessary changes to the medication regimen.
Additionally, patients with VKH may benefit from regular eye exams to check for any changes in vision or the presence of other eye conditions. Early detection and prompt treatment of any complications can help preserve vision and improve overall outcomes.
4. Supportive Care:
Alongside medical treatment, certain lifestyle modifications can help manage VKH and improve overall well-being. These include:
- Protecting the eyes from excessive sunlight by wearing sunglasses with UV protection
- Avoiding eye strain by taking regular breaks when reading or using electronic devices
- Getting adequate rest and managing stress levels
- Eating a balanced diet rich in antioxidants and nutrients that support eye health
- Seeking emotional support from friends, family, or support groups to cope with the challenges of living with a chronic condition
It is important to note that the treatment and management of VKH may vary from person to person, and the specific approach will depend on the severity of the condition and individual factors. Close collaboration between the patient, ophthalmologist, and other healthcare providers is crucial to developing an effective and personalized treatment plan.
Living with Vogt-Koyanagi-Harada Syndrome
Living with Vogt-Koyanagi-Harada Syndrome can be challenging, but with proper management and support, individuals can lead fulfilling lives. Here are some important aspects to consider when navigating life with this autoimmune disorder affecting the eyes:
1. Regular Eye Exams
It is crucial for individuals with Vogt-Koyanagi-Harada Syndrome to have regular eye exams. These exams can help monitor the progression of the disease, detect any changes in vision, and identify potential complications. Eye specialists, such as ophthalmologists, can provide specialized care and treatment options tailored to the individual’s needs.
2. Medication Adherence
Following the prescribed medication regimen is essential for managing Vogt-Koyanagi-Harada Syndrome. Medications, such as corticosteroids and immunosuppressants, help control inflammation and prevent further damage to the eyes. It is important to take medications as directed by the healthcare provider and to report any side effects or concerns promptly.
3. Lifestyle Modifications
Adopting certain lifestyle modifications can help individuals with Vogt-Koyanagi-Harada Syndrome maintain their overall health and well-being. This may include protecting the eyes from excessive sunlight by wearing sunglasses or hats, maintaining a balanced diet rich in antioxidants and nutrients, and avoiding smoking or exposure to secondhand smoke.
4. Emotional Support
Living with a chronic condition like Vogt-Koyanagi-Harada Syndrome can be emotionally challenging. It is important to seek emotional support from friends, family, or support groups. Connecting with others who have similar experiences can provide a sense of understanding and help cope with the emotional aspects of the condition.
5. Regular Follow-ups with Healthcare Providers
Regular follow-up appointments with healthcare providers are vital for monitoring the progress of Vogt-Koyanagi-Harada Syndrome and adjusting the treatment plan as needed. These appointments allow for open communication, addressing any concerns, and ensuring optimal management of the condition.
6. Education and Awareness
Education about Vogt-Koyanagi-Harada Syndrome is crucial for both individuals living with the condition and their support network. Understanding the disease, its symptoms, and treatment options can empower individuals to actively participate in their own healthcare and make informed decisions.
Remember, each person’s experience with Vogt-Koyanagi-Harada Syndrome may vary, and it is important to work closely with healthcare professionals to develop a personalized management plan. With proper care and support, individuals can lead fulfilling lives and minimize the impact of the condition on their overall well-being.
Latest Research on Vogt-Koyanagi-Harada Syndrome
Vogt-Koyanagi-Harada Syndrome (VKH) is a complex autoimmune disorder that primarily affects the eyes. Over the years, extensive research has been conducted to better understand this condition and develop more effective treatment strategies. Let’s take a look at some of the latest research findings on Vogt-Koyanagi-Harada Syndrome:
1. Genetic Factors
Recent studies have identified certain genetic factors that may contribute to the development of VKH syndrome. Researchers have found specific gene variations associated with an increased risk of developing the condition. This knowledge can help in early detection and personalized treatment approaches.
2. Immunological Mechanisms
Scientists are continuously investigating the immunological mechanisms involved in VKH syndrome. Recent research has focused on understanding the role of T-cells and their interaction with melanocytes, which are pigment-producing cells in the eyes. These studies have provided valuable insights into the underlying autoimmune processes and potential targets for therapeutic interventions.
3. Biomarkers for Diagnosis and Monitoring
Efforts are underway to identify reliable biomarkers that can aid in the diagnosis and monitoring of VKH syndrome. Researchers have explored various molecular and genetic markers that could potentially serve as indicators of disease activity and treatment response. The discovery of such biomarkers could improve the accuracy of diagnosis and help in assessing the effectiveness of different treatment approaches.
4. Novel Treatment Approaches
Advancements in research have led to the development of novel treatment approaches for VKH syndrome. Targeted therapies, such as biologics and immunomodulatory drugs, are being investigated to specifically inhibit the autoimmune response and reduce inflammation in the eyes. Additionally, gene therapy and stem cell transplantation techniques are being explored as potential future treatment options.
5. Improved Disease Management
Research efforts have also focused on improving the overall management of VKH syndrome. Studies have evaluated the effectiveness of multidisciplinary care approaches involving ophthalmologists, rheumatologists, and other healthcare professionals to provide comprehensive treatment and support to patients. Additionally, the development of patient education programs and support groups can help individuals with VKH syndrome better cope with the challenges posed by the condition.
As research in the field of Vogt-Koyanagi-Harada Syndrome continues to progress, it holds the promise of further enhancing our understanding of the condition and improving patient outcomes. These advancements pave the way for more targeted and personalized treatment strategies, ultimately offering hope to individuals affected by this autoimmune disorder affecting the eyes.
Frequently Asked Questions about Vogt-Koyanagi-Harada Syndrome
What is Vogt-Koyanagi-Harada Syndrome?
Vogt-Koyanagi-Harada Syndrome (VKH) is a rare autoimmune disorder that primarily affects the eyes but can also involve other parts of the body. It is characterized by inflammation of the uvea, which is the middle layer of the eye that contains the iris, ciliary body, and choroid. VKH is thought to result from an abnormal immune response that mistakenly targets the melanocytes, cells responsible for producing pigment in the eyes, skin, and hair.
How does Vogt-Koyanagi-Harada Syndrome affect the eyes?
VKH primarily affects the eyes and can lead to a variety of symptoms including blurred vision, sensitivity to light, redness, eye pain, and excessive tearing. In some cases, VKH can also cause vision loss or blindness if left untreated. The inflammation in VKH can affect multiple parts of the eye, including the retina, optic nerve, and the fluid-filled spaces within the eye.
What are the symptoms of Vogt-Koyanagi-Harada Syndrome?
The symptoms of VKH can vary from person to person, but commonly include:
- Blurred or decreased vision
- Eye redness and pain
- Sensitivity to light
- Excessive tearing
- Floaters in the field of vision
- Changes in color vision
- Hearing loss
- Headaches
- Skin and hair changes, such as whitening or graying
What causes Vogt-Koyanagi-Harada Syndrome?
The exact cause of VKH is unknown, but it is believed to be an autoimmune disorder, which means that the body’s immune system mistakenly attacks its own healthy cells. Genetic factors are thought to play a role in predisposing individuals to develop VKH, and certain ethnic groups, such as Asians, Native Americans, and Hispanics, have a higher risk of developing the syndrome.
How is Vogt-Koyanagi-Harada Syndrome diagnosed?
Diagnosing VKH involves a combination of medical history evaluation, eye examinations, and diagnostic tests. An ophthalmologist will assess the symptoms, perform a comprehensive eye examination, and may order additional tests such as an optical coherence tomography (OCT) scan, fluorescein angiography, or an ultrasound of the eye to evaluate the extent of inflammation and damage.
What are the treatment options for Vogt-Koyanagi-Harada Syndrome?
The goal of treatment for VKH is to reduce inflammation, preserve vision, and prevent complications. Treatment typically involves a combination of corticosteroids to suppress the immune response, immunosuppressive drugs to control inflammation, and sometimes additional medications to manage symptoms such as pain or increased eye pressure.
Can Vogt-Koyanagi-Harada Syndrome be cured?
Currently, there is no cure for VKH. However, with early diagnosis and appropriate treatment, the majority of individuals with VKH can achieve remission and maintain good vision. Long-term follow-up with an ophthalmologist is necessary to monitor for any recurrence of symptoms or complications.
Is Vogt-Koyanagi-Harada Syndrome a progressive disease?
VKH is typically characterized by an acute onset of symptoms, followed by an inflammatory stage and a subsequent convalescent stage. Without proper treatment, VKH can progress and lead to permanent vision loss or other complications. However, with early and appropriate treatment, the disease can be managed effectively, and the prognosis is generally favorable.
Is Vogt-Koyanagi-Harada Syndrome hereditary?
While the exact cause of VKH is unknown, there is evidence to suggest a genetic predisposition to the syndrome. Certain genetic variations have been associated with an increased risk of developing VKH, and individuals with a family history of the disorder may have a higher likelihood of developing it themselves. However, VKH is not solely determined by genetics, and other factors, such as environmental triggers, may also contribute to its development.
Are there any ongoing research studies or clinical trials for Vogt-Koyanagi-Harada Syndrome?
Yes, there are ongoing research studies and clinical trials aimed at further understanding the underlying causes of VKH, improving diagnostic methods, and developing more targeted and effective treatments. Participation in clinical trials may be an option for individuals with VKH who are interested in contributing to scientific advancements and potentially accessing new treatment options.